Tuesday Poster Session
Category: Interventional Endoscopy
P4502 - Fenestrated Gallbladders and Bile Leaks: An Upfront Endoscopic Approach to Improve Outcomes
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Alexander T. Miller, MD
Dartmouth-Hitchcock Medical Center
Lebanon, NH
Presenting Author(s)
Alexander Miller, MD1, Obaida Dairi, DO1, Timothy B.. Gardner, MD, MS2
1Dartmouth-Hitchcock Medical Center, Lebanon, NH; 2Dartmouth Hitchcock Medical Center, Lebanon, NH
Introduction: Fenestrated cholecystectomy is one strategy that surgeons consider during a difficult cholecystectomy when a total laparoscopic or open cholecystectomy is not possible. However, fenestrated cholecystectomy is known to increase the risk of bile leak, with a bile leak occurring in 12.2%1 of patients who receive a fenestrated cholecystectomy compared to rates ranging from 0.25%-2%2 for all other forms of cholecystectomy. Thus, being able to identify an endoscopic intervention that may improve outcomes (specifically bile leak resolution) in patients who receive a fenestrated cholecystectomy is necessary.
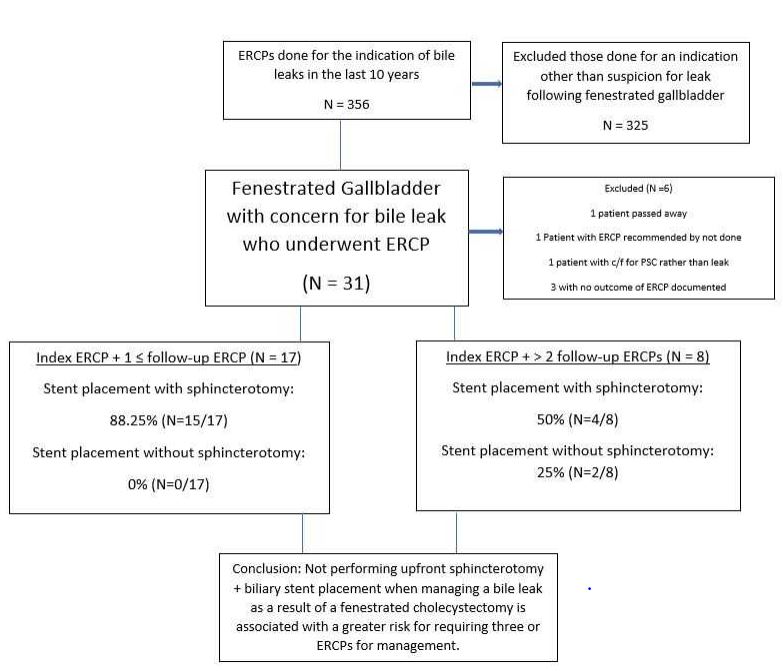
Methods: We retrospectively reviewed 356 cases of bile leaks that occurred over a ten-year period from 2014-2024. We excluded 325 cases that did not involve a fenestrated cholecystectomy. We divided the fenestrated cholecystectomy cases into those requiring two or less ERCPs for management of the bile leak versus those requiring three or more ERCPs. We then compared the patient characteristics and endoscopic interventions between the two groups with the goal of identifying an upfront endoscopic approach that would improve outcomes. Our primary outcome was resolution of the bile leak requiring the least amount of repeat intervention.
Results: Out of 31 bile leaks resulting from a fenestrated cholecystectomy, six were excluded (reasons noted in figure 1). Of the remaining 25, 68% had two or less ERCPs, while 32% had three or more ERCPs. We did not observe a difference in age, gender, or type of fenestrated cholecystectomy performed. We observed that patients that had three or more ERCPs required multiple interventions as a result of initial biliary stent placement alone without a biliary sphincterotomy when compared with two or less ERCPs, 25% vs. 0% (p=0.0933). We also observed a trend near statistical significance that those with two or less ERCPs compared to the three or more ERCPs were managed upfront with biliary stent placement in conjunction with a sphincterotomy, 88.25% vs 50% (p=0.0593).
Discussion: Patients with a bile leak following fenestrated cholecystectomy are potentially at risk for multiple recurrent endoscopic intervention (specifically, more than two ERCPs) if they are not treated upfront with a combination of a biliary stent placement combined with sphincterotomy. Randomized control trials with an increased sample size will be necessary to confirm this trend.
1. Toro A et al., World J Emerg Surg, 2021 Sep 8, 16(1):45
2. Brunt LM et al., Ann Surg, 2020 Jul, 272(1):3-23
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alexander Miller, MD1, Obaida Dairi, DO1, Timothy B.. Gardner, MD, MS2. P4502 - Fenestrated Gallbladders and Bile Leaks: An Upfront Endoscopic Approach to Improve Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Dartmouth-Hitchcock Medical Center, Lebanon, NH; 2Dartmouth Hitchcock Medical Center, Lebanon, NH
Introduction: Fenestrated cholecystectomy is one strategy that surgeons consider during a difficult cholecystectomy when a total laparoscopic or open cholecystectomy is not possible. However, fenestrated cholecystectomy is known to increase the risk of bile leak, with a bile leak occurring in 12.2%1 of patients who receive a fenestrated cholecystectomy compared to rates ranging from 0.25%-2%2 for all other forms of cholecystectomy. Thus, being able to identify an endoscopic intervention that may improve outcomes (specifically bile leak resolution) in patients who receive a fenestrated cholecystectomy is necessary.
Methods: We retrospectively reviewed 356 cases of bile leaks that occurred over a ten-year period from 2014-2024. We excluded 325 cases that did not involve a fenestrated cholecystectomy. We divided the fenestrated cholecystectomy cases into those requiring two or less ERCPs for management of the bile leak versus those requiring three or more ERCPs. We then compared the patient characteristics and endoscopic interventions between the two groups with the goal of identifying an upfront endoscopic approach that would improve outcomes. Our primary outcome was resolution of the bile leak requiring the least amount of repeat intervention.
Results: Out of 31 bile leaks resulting from a fenestrated cholecystectomy, six were excluded (reasons noted in figure 1). Of the remaining 25, 68% had two or less ERCPs, while 32% had three or more ERCPs. We did not observe a difference in age, gender, or type of fenestrated cholecystectomy performed. We observed that patients that had three or more ERCPs required multiple interventions as a result of initial biliary stent placement alone without a biliary sphincterotomy when compared with two or less ERCPs, 25% vs. 0% (p=0.0933). We also observed a trend near statistical significance that those with two or less ERCPs compared to the three or more ERCPs were managed upfront with biliary stent placement in conjunction with a sphincterotomy, 88.25% vs 50% (p=0.0593).
Discussion: Patients with a bile leak following fenestrated cholecystectomy are potentially at risk for multiple recurrent endoscopic intervention (specifically, more than two ERCPs) if they are not treated upfront with a combination of a biliary stent placement combined with sphincterotomy. Randomized control trials with an increased sample size will be necessary to confirm this trend.
1. Toro A et al., World J Emerg Surg, 2021 Sep 8, 16(1):45
2. Brunt LM et al., Ann Surg, 2020 Jul, 272(1):3-23
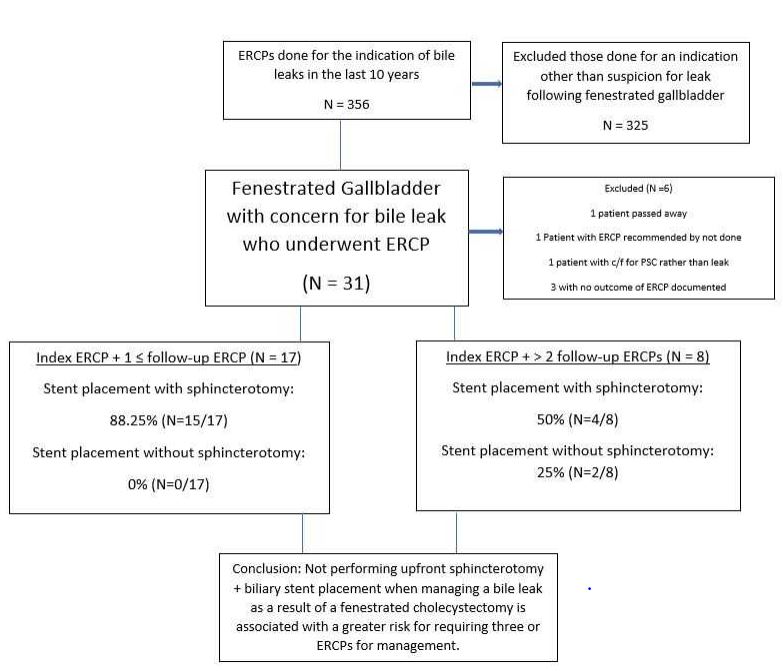
Figure: Flow Chart of Excluded Cases and Distribution of Included Cases
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Alexander Miller indicated no relevant financial relationships.
Obaida Dairi indicated no relevant financial relationships.
Timothy Gardner indicated no relevant financial relationships.
Alexander Miller, MD1, Obaida Dairi, DO1, Timothy B.. Gardner, MD, MS2. P4502 - Fenestrated Gallbladders and Bile Leaks: An Upfront Endoscopic Approach to Improve Outcomes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
