Tuesday Poster Session
Category: Interventional Endoscopy
P4529 - Type 1C Choledochal Cyst With Recurrent CBD Dilation After Roux-en-Y Hepaticojejunostomy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ikjot Singh, MD
University at Buffalo
Buffalo, NY
Presenting Author(s)
Ikjot Singh, MD1, Ahmed Gabr, 2, Nariman Hossein-Javaheri, DO1, Naren Nallapeta, MD1, Clive J. Miranda, DO, MSc3, Henry Klos, MD1, Mayada Ismail, MD1
1University at Buffalo, Buffalo, NY; 2New York Medical College, Valhalla, NY; 3CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Choledochal cysts are rare, with an incidence of 1 in 150,000 individuals, most common in Asia. Due to very high risk of malignant transformation, they require early total surgical resection of the biliary structures, with either Roux-en-Y hepaticojejunostomy or hepaticoduodenostomy.
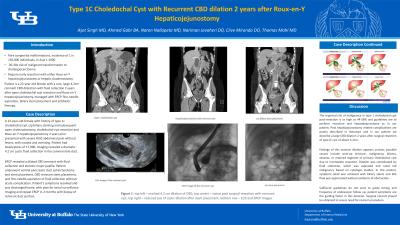
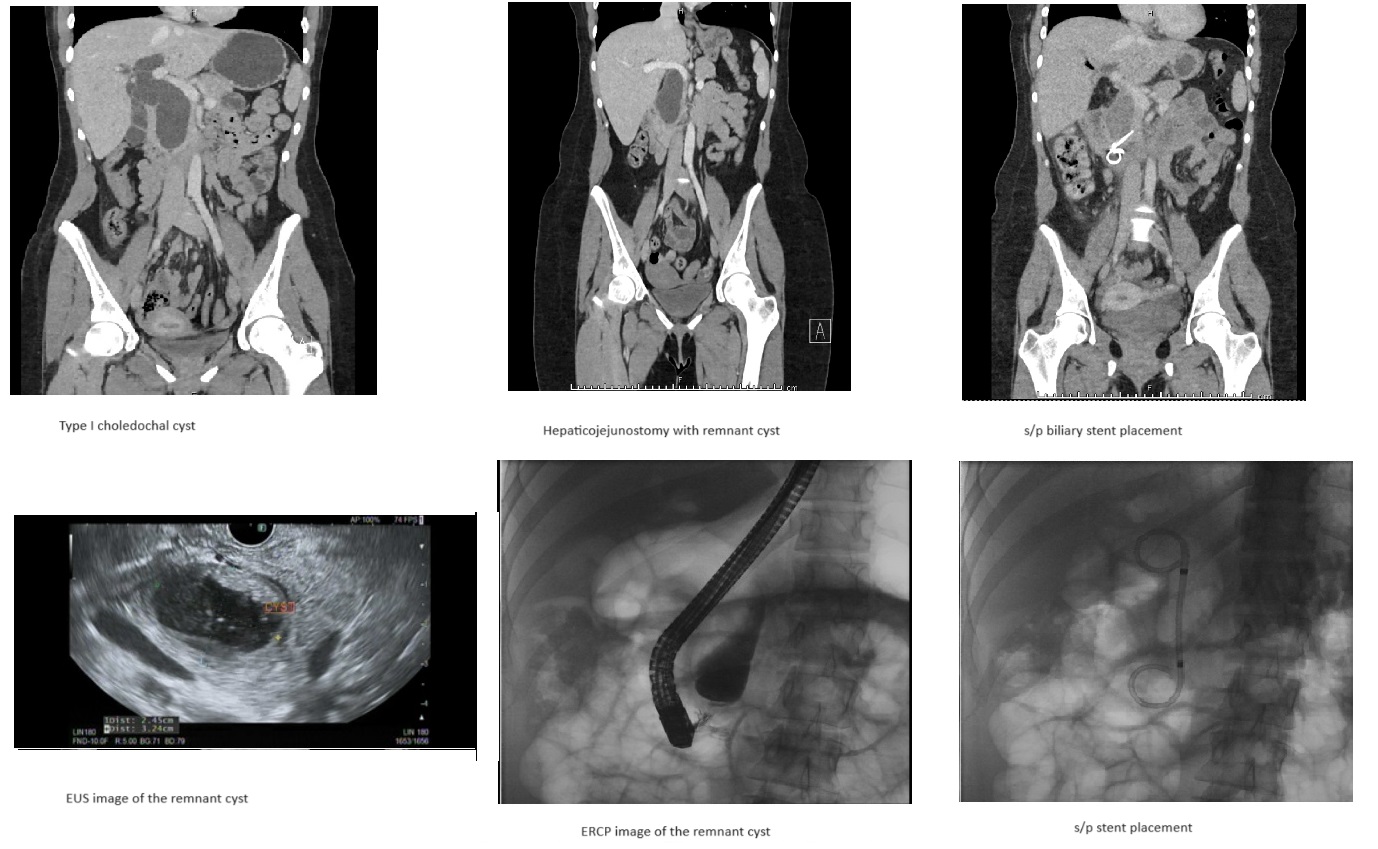
In this case report we describe a young female with a rare, large 4.2cm remnant CBD dilatation with fluid collection 2 years after open choledochal cyst resection and Roux-en-Y hepaticojejunostomy, managed with fine-needle aspiration, and biliary stent placement.
Case Description/Methods: A 22-year-old female with history of type 1c choledochal cyst s/p biliary stenting and subsequent open cholecystectomy, choledochal cyst resection and Roux-en-Y hepaticojejunostomy 2 years prior presented with severe RUQ abdominal pain without fevers, with nausea and vomiting. Patient had leukocytosis of 17,900, imaging revealed a dramatic 4.2 cm CBD dilation. Repeat ERCP revealed a dilated CBD remnant with fluid collection and stenotic major papilla. Patient underwent ventral pancreatic duct sphincterotomy and stent placement, CBD remnant stent placement, and fine-needle aspiration of fluid collection without acute complication. Her symptoms resolved and she was discharged home.
Discussion: The reported risk of malignancy in type 1 choledochal cyst ranges from 2.5-2.8% and guidelines are to perform early resection and hepaticojejunostomy as in our patient. Post hepaticojejunostomy related complications are poorly described in literature and here we describe a large CBD dilation 2 years post-operation of 4.2cm. The etiology of this massive dilation appears unclear, possible causes include post-op stricture, malignancy, biloma, abscess, or retained segment of primary choledochal cyst due to incomplete resection. Here, dilation was complicated by fluid collection, which was aspirated and ruled out malignancy based on cytologic studies. In this case, symptomatic relief was achieved with biliary stents and bile flow was appreciated without evidence of obstruction. Sufficient guidelines do not exist to guide decisions on timing and frequency of endoscopic follow-up, patient symptoms and expert opinion are the guiding factor in this decision. Surgical consult should be obtained to assess the need for revision procedure.
Disclosures:
Ikjot Singh, MD1, Ahmed Gabr, 2, Nariman Hossein-Javaheri, DO1, Naren Nallapeta, MD1, Clive J. Miranda, DO, MSc3, Henry Klos, MD1, Mayada Ismail, MD1. P4529 - Type 1C Choledochal Cyst With Recurrent CBD Dilation After Roux-en-Y Hepaticojejunostomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2New York Medical College, Valhalla, NY; 3CHI Health Creighton University Medical Center, Omaha, NE
Introduction: Choledochal cysts are rare, with an incidence of 1 in 150,000 individuals, most common in Asia. Due to very high risk of malignant transformation, they require early total surgical resection of the biliary structures, with either Roux-en-Y hepaticojejunostomy or hepaticoduodenostomy.
In this case report we describe a young female with a rare, large 4.2cm remnant CBD dilatation with fluid collection 2 years after open choledochal cyst resection and Roux-en-Y hepaticojejunostomy, managed with fine-needle aspiration, and biliary stent placement.
Case Description/Methods: A 22-year-old female with history of type 1c choledochal cyst s/p biliary stenting and subsequent open cholecystectomy, choledochal cyst resection and Roux-en-Y hepaticojejunostomy 2 years prior presented with severe RUQ abdominal pain without fevers, with nausea and vomiting. Patient had leukocytosis of 17,900, imaging revealed a dramatic 4.2 cm CBD dilation. Repeat ERCP revealed a dilated CBD remnant with fluid collection and stenotic major papilla. Patient underwent ventral pancreatic duct sphincterotomy and stent placement, CBD remnant stent placement, and fine-needle aspiration of fluid collection without acute complication. Her symptoms resolved and she was discharged home.
Discussion: The reported risk of malignancy in type 1 choledochal cyst ranges from 2.5-2.8% and guidelines are to perform early resection and hepaticojejunostomy as in our patient. Post hepaticojejunostomy related complications are poorly described in literature and here we describe a large CBD dilation 2 years post-operation of 4.2cm. The etiology of this massive dilation appears unclear, possible causes include post-op stricture, malignancy, biloma, abscess, or retained segment of primary choledochal cyst due to incomplete resection. Here, dilation was complicated by fluid collection, which was aspirated and ruled out malignancy based on cytologic studies. In this case, symptomatic relief was achieved with biliary stents and bile flow was appreciated without evidence of obstruction. Sufficient guidelines do not exist to guide decisions on timing and frequency of endoscopic follow-up, patient symptoms and expert opinion are the guiding factor in this decision. Surgical consult should be obtained to assess the need for revision procedure.
Figure: Type 1C choledochal cyst s/p surgical resection 2 years prior with development of large 4.2cm CBD dilation
Disclosures:
Ikjot Singh indicated no relevant financial relationships.
Ahmed Gabr indicated no relevant financial relationships.
Nariman Hossein-Javaheri indicated no relevant financial relationships.
Naren Nallapeta indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Henry Klos indicated no relevant financial relationships.
Mayada Ismail indicated no relevant financial relationships.
Ikjot Singh, MD1, Ahmed Gabr, 2, Nariman Hossein-Javaheri, DO1, Naren Nallapeta, MD1, Clive J. Miranda, DO, MSc3, Henry Klos, MD1, Mayada Ismail, MD1. P4529 - Type 1C Choledochal Cyst With Recurrent CBD Dilation After Roux-en-Y Hepaticojejunostomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
