Tuesday Poster Session
Category: Interventional Endoscopy
P4530 - A "Bloody" Obstruction: A Case of Duodenal Hematoma Treated With Endoscopic Balloon Dilatation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AA
Aysha Aslam, MD
University of Iowa Hospitals & Clinics
Iowa City, IA
Presenting Author(s)
Aysha Aslam, MD, Rami El Abiad, MD
University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Duodenal hematomas (DH) are rare complications of blunt abdominal trauma, with symptom severity reflecting the degree of luminal narrowing. Without perforation, management revolves around nasogastric (NG) decompression and parenteral nutrition or Naso jejunal tube feeding. Spontaneous resolution is often protracted, and symptoms may linger for weeks, delaying adequate oral intake. We present a case of gastric outlet obstruction (GOO) due to a DH who failed conservative management and was treated with endoscopic balloon dilation
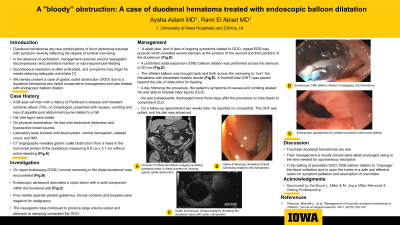
Case Description/Methods: A 68-year-old man with a history of Parkinson's disease and transient ischemic attack on Clopidogrel presented with nausea, vomiting (N/V), and loss of appetite post abdominal trauma related to a fall. His vital signs were stable. On physical examination, he had mild abdominal distension and hyperactive bowel sounds. Lab tests showed mild leukocytosis, normal hemoglobin, platelets, and INR. CT angiography revealed GOO from a mass in the horizontal portion of the duodenum measuring 6.9 x 5.1 cm without active bleeding (Fig.1). On upper endoscopy (EGD), luminal narrowing in the distal duodenum was noted (Fig.2). EUS described a cystic lesion with a solid component in the duodenal wall (Fig.3). Fine needle aspirate yielded gelatinous, bloody contents and biopsies were negative for malignancy. The NG continued to produce large volume output, and attempts at clamping unmasked the GOO. A week later, with ongoing symptoms related to GOO, repeat EGD was pursued, which revealed severe stenosis at the junction of the 2nd and 3rd portions of the duodenum. A controlled radial expansion (CRE) balloon dilation was performed across the stenosis to 20 mm (Fig.4). The inflated balloon was brought back and forth across the narrowing to "iron" the hematoma with notable dilatation (Fig.5). A Duboff tube (DHT) was placed beyond the site of obstruction for feeding. A day after the procedure, the patient's N/V abated, could tolerate clear liquids, and was discharged home 3 days after the procedure on tube feeds. On a follow-up appointment 2 weeks later, he was able to tolerate a full liquid diet without symptoms and the DHT tube was removed.
Discussion: Traumatic DH is rare. Their management is primarily conservative, albeit prolonged, owing to the time needed for spontaneous resorption. In persistent GOO, CRE balloon dilation to “massage” the blood collection to open the lumen is a safe and effective option for symptom palliation and resumption of oral intake.

Disclosures:
Aysha Aslam, MD, Rami El Abiad, MD. P4530 - A "Bloody" Obstruction: A Case of Duodenal Hematoma Treated With Endoscopic Balloon Dilatation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Duodenal hematomas (DH) are rare complications of blunt abdominal trauma, with symptom severity reflecting the degree of luminal narrowing. Without perforation, management revolves around nasogastric (NG) decompression and parenteral nutrition or Naso jejunal tube feeding. Spontaneous resolution is often protracted, and symptoms may linger for weeks, delaying adequate oral intake. We present a case of gastric outlet obstruction (GOO) due to a DH who failed conservative management and was treated with endoscopic balloon dilation
Case Description/Methods: A 68-year-old man with a history of Parkinson's disease and transient ischemic attack on Clopidogrel presented with nausea, vomiting (N/V), and loss of appetite post abdominal trauma related to a fall. His vital signs were stable. On physical examination, he had mild abdominal distension and hyperactive bowel sounds. Lab tests showed mild leukocytosis, normal hemoglobin, platelets, and INR. CT angiography revealed GOO from a mass in the horizontal portion of the duodenum measuring 6.9 x 5.1 cm without active bleeding (Fig.1). On upper endoscopy (EGD), luminal narrowing in the distal duodenum was noted (Fig.2). EUS described a cystic lesion with a solid component in the duodenal wall (Fig.3). Fine needle aspirate yielded gelatinous, bloody contents and biopsies were negative for malignancy. The NG continued to produce large volume output, and attempts at clamping unmasked the GOO. A week later, with ongoing symptoms related to GOO, repeat EGD was pursued, which revealed severe stenosis at the junction of the 2nd and 3rd portions of the duodenum. A controlled radial expansion (CRE) balloon dilation was performed across the stenosis to 20 mm (Fig.4). The inflated balloon was brought back and forth across the narrowing to "iron" the hematoma with notable dilatation (Fig.5). A Duboff tube (DHT) was placed beyond the site of obstruction for feeding. A day after the procedure, the patient's N/V abated, could tolerate clear liquids, and was discharged home 3 days after the procedure on tube feeds. On a follow-up appointment 2 weeks later, he was able to tolerate a full liquid diet without symptoms and the DHT tube was removed.
Discussion: Traumatic DH is rare. Their management is primarily conservative, albeit prolonged, owing to the time needed for spontaneous resorption. In persistent GOO, CRE balloon dilation to “massage” the blood collection to open the lumen is a safe and effective option for symptom palliation and resumption of oral intake.

Figure: Figure 1. Coronal CT Abdomen/Pelvis imaging revealing duodenal mass in distal duodenum causing gastric outlet obstruction.
Figure 2: Upper endoscopy revealing luminal narrowing related to the hematoma.
Figure 3: Upper endoscopic ultrasonography revealing the duodenal mass with cystic component.
Figure 4: Endoscopic CRE balloon dilation “massaging: the hematoma
Figure 5: Endoscopic appearance of a patent duodenal lumen post dilation
Figure 2: Upper endoscopy revealing luminal narrowing related to the hematoma.
Figure 3: Upper endoscopic ultrasonography revealing the duodenal mass with cystic component.
Figure 4: Endoscopic CRE balloon dilation “massaging: the hematoma
Figure 5: Endoscopic appearance of a patent duodenal lumen post dilation
Disclosures:
Aysha Aslam indicated no relevant financial relationships.
Rami El Abiad indicated no relevant financial relationships.
Aysha Aslam, MD, Rami El Abiad, MD. P4530 - A "Bloody" Obstruction: A Case of Duodenal Hematoma Treated With Endoscopic Balloon Dilatation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

