Tuesday Poster Session
Category: Interventional Endoscopy
P4533 - Prostate Cancer Recurrence in the Rectum Diagnosed by Endoscopic Ultrasound-Guided Fine Needle Biopsy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DM
Destinee Morris, MD
Tripler Army Medical Center
Honolulu, HI
Presenting Author(s)
Destinee Morris, MD, Andrew Landau, MD, Yula Geniza, MD, John Lee, MD, Pedro Manibusan, DO, MBA
Tripler Army Medical Center, Honolulu, HI
Introduction: Prostate cancer is the second most diagnosed cancer in the world. Definitive diagnosis requires tissue biopsy with pathologic evaluation which is crucial not only for staging, but also to guide treatment strategies. Transrectal and transperineal biopsy are the two most common techniques for diagnosis. However, in more complicated cases, there may be a role for endoscopic ultrasound (EUS)-guided rectal biopsy when diagnosis of recurrent or metastatic prostate cancer is suspected. While typically used to diagnose pathologies in the upper gastrointestinal tract, transrectal EUS fine needle aspiration (FNA) is emerging as a safe, effective, and accurate technique for diagnosis of space-occupying lesions in the rectum. We present a case of prostate cancer recurrence diagnosed by EUS-guided rectal biopsy by the gastroenterology service.
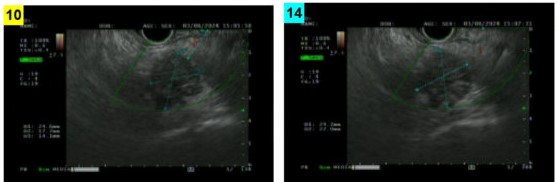
Case Description/Methods: A 74 year-old male with leukemia in remission and remote history of prostate cancer status post prostatectomy presented to radiology for routine PET/CT for disease monitoring. The study showed a 2 cm prominent intense hypermetabolic focus in the right peri-rectosigmoid region. He was referred to gastroenterology for EUS with FNA and fine needle biopsy (FNB). Limited colonoscopy was performed to gauge stool burden and mark the rectal wall. Endoscopic ultrasound was notable for a heterogenous, irregular-shaped lesion with poorly defined borders in the peri-rectal space measuring 1.5 cm x 1.8 cm. FNA and FNB were performed for which histopathology revealed adenocarcinoma of prostate origin. Upon further chart review, the patient had positive margins after prostatectomy and despite PSA recurrence 10 years later, no salvage therapy was attempted. Shared decision was made with the patinent's medical team for treatment with radiation and androgen deprivation therapy.
Discussion: This case presents an alternative diagnostic tool for peri-rectal lesions to include those involving patients at risk for recurrent or metastatic prostate cancer. Though rectosigmoid involvement of metastatic prostate cancer is rare, prostate cancer recurrence should be on the differential for hypermetabolic lesions in the rectosigmoid region for patients with history of prostate cancer, especially in this particular case in which the patient received incomplete treatment. Although diagnosis of prostate cancer is typically made by a urologist, there may be a role for the gastroenterologist with advanced training to aid in diagnosis of more complex cases.
Disclosures:
Destinee Morris, MD, Andrew Landau, MD, Yula Geniza, MD, John Lee, MD, Pedro Manibusan, DO, MBA. P4533 - Prostate Cancer Recurrence in the Rectum Diagnosed by Endoscopic Ultrasound-Guided Fine Needle Biopsy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Tripler Army Medical Center, Honolulu, HI
Introduction: Prostate cancer is the second most diagnosed cancer in the world. Definitive diagnosis requires tissue biopsy with pathologic evaluation which is crucial not only for staging, but also to guide treatment strategies. Transrectal and transperineal biopsy are the two most common techniques for diagnosis. However, in more complicated cases, there may be a role for endoscopic ultrasound (EUS)-guided rectal biopsy when diagnosis of recurrent or metastatic prostate cancer is suspected. While typically used to diagnose pathologies in the upper gastrointestinal tract, transrectal EUS fine needle aspiration (FNA) is emerging as a safe, effective, and accurate technique for diagnosis of space-occupying lesions in the rectum. We present a case of prostate cancer recurrence diagnosed by EUS-guided rectal biopsy by the gastroenterology service.
Case Description/Methods: A 74 year-old male with leukemia in remission and remote history of prostate cancer status post prostatectomy presented to radiology for routine PET/CT for disease monitoring. The study showed a 2 cm prominent intense hypermetabolic focus in the right peri-rectosigmoid region. He was referred to gastroenterology for EUS with FNA and fine needle biopsy (FNB). Limited colonoscopy was performed to gauge stool burden and mark the rectal wall. Endoscopic ultrasound was notable for a heterogenous, irregular-shaped lesion with poorly defined borders in the peri-rectal space measuring 1.5 cm x 1.8 cm. FNA and FNB were performed for which histopathology revealed adenocarcinoma of prostate origin. Upon further chart review, the patient had positive margins after prostatectomy and despite PSA recurrence 10 years later, no salvage therapy was attempted. Shared decision was made with the patinent's medical team for treatment with radiation and androgen deprivation therapy.
Discussion: This case presents an alternative diagnostic tool for peri-rectal lesions to include those involving patients at risk for recurrent or metastatic prostate cancer. Though rectosigmoid involvement of metastatic prostate cancer is rare, prostate cancer recurrence should be on the differential for hypermetabolic lesions in the rectosigmoid region for patients with history of prostate cancer, especially in this particular case in which the patient received incomplete treatment. Although diagnosis of prostate cancer is typically made by a urologist, there may be a role for the gastroenterologist with advanced training to aid in diagnosis of more complex cases.
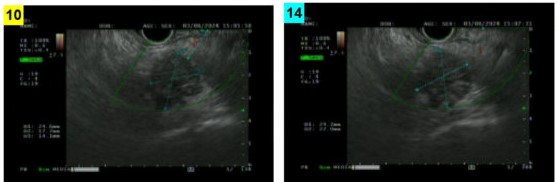
Figure: Irregular-shaped, heterogenous peri-rectal lesion noted on linear examination, measuring about 1.5 cm x 1.8 cm
Disclosures:
Destinee Morris indicated no relevant financial relationships.
Andrew Landau indicated no relevant financial relationships.
Yula Geniza indicated no relevant financial relationships.
John Lee indicated no relevant financial relationships.
Pedro Manibusan indicated no relevant financial relationships.
Destinee Morris, MD, Andrew Landau, MD, Yula Geniza, MD, John Lee, MD, Pedro Manibusan, DO, MBA. P4533 - Prostate Cancer Recurrence in the Rectum Diagnosed by Endoscopic Ultrasound-Guided Fine Needle Biopsy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
