Tuesday Poster Session
Category: Interventional Endoscopy
P4537 - Early Stent Migration Leading to Duodenal Perforation Post-Cholecystectomy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Patricia Zarza-Gulino, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Patricia Zarza-Gulino, MD, Victor Udechukwu, MD, Enrique F. Martinez Trevino, MD, Alejandro J. Nieto Dominguez, MD, Bhanu Siva Mohan Pinnam, MD, Robert Kwei Nsoro, MD
John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Few cases of duodenal perforation due to a migrated biliary stent have been reported in the literature. We present a case of early stent migration complicated by duodenal perforation after laparoscopic cholecystectomy.
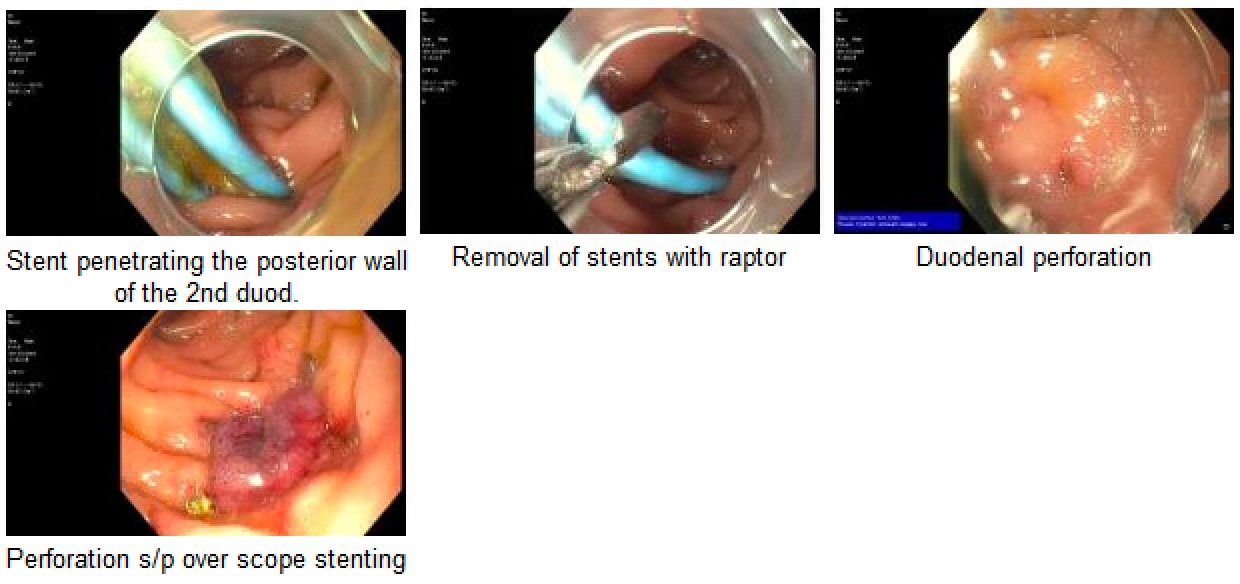
Case Description/Methods: A 26-year-old female with no significant medical history presented with 2 weeks of right upper quadrant pain, jaundice, and dark urine. Initial labs revealed cholestatic pattern associated with elevated transaminases. Abdominal CT and ultrasound indicated acute cholecystitis, proximal dilation of the common bile duct, intrahepatic biliary ducts, and a large stone in the gallbladder neck, suggesting Mirizzi syndrome. ERCP confirmed narrowing of the common hepatic duct/bifurcation with dilated intrahepatic ducts. A 7Fr 15cm stent was placed in the left hepatic duct and a 7Fr 12cm stent in the right anterior branch. Post-procedure, patient developed severe abdominal pain and bilious emesis. Work up revealed a normal lipase and CT abdomen. Three days later, symptoms improved and she underwent laparoscopic cholecystectomy with partial gallbladder resection due to severe adhesions. Postoperative course was complicated by ileus, abdominal discomfort, and persistent abnormal LFTs. A repeat CT on POD 4 showed a retroperitoneal fluid collection with biliary stents in place. Interventional radiology drainage revealed yellow-green fluid. Due to persistent abnormal LFTs, repeat EGD revealed two migrated stents: one in the duodenal lumen and the other penetrating the posterior duodenal wall. The penetrating stent was removed. Perforation was closed with an OVESCO clip. A 1 cm common bile duct stricture was noted, and a single stent was placed in the left main hepatic duct. A small bowel follow-through three days later showed no duodenal leak.
Discussion: Endoscopic biliary stent placement is a common intervention for benign or malignant biliary obstructions. Approximately 14% of cases experience stent migration, with a 1% incidence of organ perforation, notably in the duodenum. The precise factors predisposing to early stent migration remain uncertain. Reported cases highlighted the use of a straight stent, excessive stent length, or retention of the proximal end of the stent in the CBD as possible causes. In our case, stent migration occurred after laparoscopic cholecystectomy. We want to emphasize the role of early ERCP in detecting stent complications in patients presenting with severe abdominal pain after procedure despite normal lipase and unspecific CT findings.
Disclosures:
Patricia Zarza-Gulino, MD, Victor Udechukwu, MD, Enrique F. Martinez Trevino, MD, Alejandro J. Nieto Dominguez, MD, Bhanu Siva Mohan Pinnam, MD, Robert Kwei Nsoro, MD. P4537 - Early Stent Migration Leading to Duodenal Perforation Post-Cholecystectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
John H. Stroger, Jr. Hospital of Cook County, Chicago, IL
Introduction: Few cases of duodenal perforation due to a migrated biliary stent have been reported in the literature. We present a case of early stent migration complicated by duodenal perforation after laparoscopic cholecystectomy.
Case Description/Methods: A 26-year-old female with no significant medical history presented with 2 weeks of right upper quadrant pain, jaundice, and dark urine. Initial labs revealed cholestatic pattern associated with elevated transaminases. Abdominal CT and ultrasound indicated acute cholecystitis, proximal dilation of the common bile duct, intrahepatic biliary ducts, and a large stone in the gallbladder neck, suggesting Mirizzi syndrome. ERCP confirmed narrowing of the common hepatic duct/bifurcation with dilated intrahepatic ducts. A 7Fr 15cm stent was placed in the left hepatic duct and a 7Fr 12cm stent in the right anterior branch. Post-procedure, patient developed severe abdominal pain and bilious emesis. Work up revealed a normal lipase and CT abdomen. Three days later, symptoms improved and she underwent laparoscopic cholecystectomy with partial gallbladder resection due to severe adhesions. Postoperative course was complicated by ileus, abdominal discomfort, and persistent abnormal LFTs. A repeat CT on POD 4 showed a retroperitoneal fluid collection with biliary stents in place. Interventional radiology drainage revealed yellow-green fluid. Due to persistent abnormal LFTs, repeat EGD revealed two migrated stents: one in the duodenal lumen and the other penetrating the posterior duodenal wall. The penetrating stent was removed. Perforation was closed with an OVESCO clip. A 1 cm common bile duct stricture was noted, and a single stent was placed in the left main hepatic duct. A small bowel follow-through three days later showed no duodenal leak.
Discussion: Endoscopic biliary stent placement is a common intervention for benign or malignant biliary obstructions. Approximately 14% of cases experience stent migration, with a 1% incidence of organ perforation, notably in the duodenum. The precise factors predisposing to early stent migration remain uncertain. Reported cases highlighted the use of a straight stent, excessive stent length, or retention of the proximal end of the stent in the CBD as possible causes. In our case, stent migration occurred after laparoscopic cholecystectomy. We want to emphasize the role of early ERCP in detecting stent complications in patients presenting with severe abdominal pain after procedure despite normal lipase and unspecific CT findings.
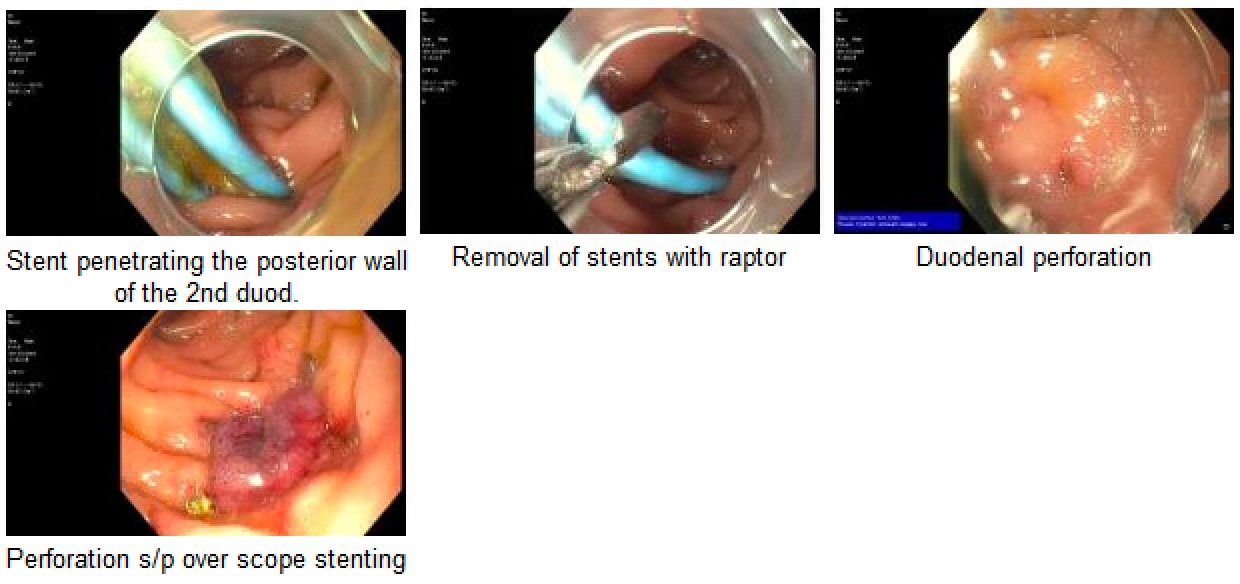
Figure: Endoscopic intervention
Disclosures:
Patricia Zarza-Gulino indicated no relevant financial relationships.
Victor Udechukwu indicated no relevant financial relationships.
Enrique Martinez Trevino indicated no relevant financial relationships.
Alejandro Nieto Dominguez indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Robert Kwei Nsoro indicated no relevant financial relationships.
Patricia Zarza-Gulino, MD, Victor Udechukwu, MD, Enrique F. Martinez Trevino, MD, Alejandro J. Nieto Dominguez, MD, Bhanu Siva Mohan Pinnam, MD, Robert Kwei Nsoro, MD. P4537 - Early Stent Migration Leading to Duodenal Perforation Post-Cholecystectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
