Tuesday Poster Session
Category: Interventional Endoscopy
P4541 - Neuroendocrine Tumor of the Ampulla of Vater: A Rare Cause of Biliary Obstruction
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Erika A. Tsuchiyose, BA
Tufts University School of Medicine
Boston, MA
Presenting Author(s)
Award: Presidential Poster Award
Erika A. Tsuchiyose, BA1, Michael Talanian, MD2, Erik Holzwanger, MD2
1Tufts University School of Medicine, Boston, MA; 2Tufts Medical Center, Boston, MA
Introduction: Neuroendocrine tumor (NET) of the ampulla of Vater (AV) is an exceedingly rare cause of biliary obstruction. We present an unusual case of a subepithelial ampullary NET leading to biliary obstruction diagnosed with endoscopic ultrasound (EUS).
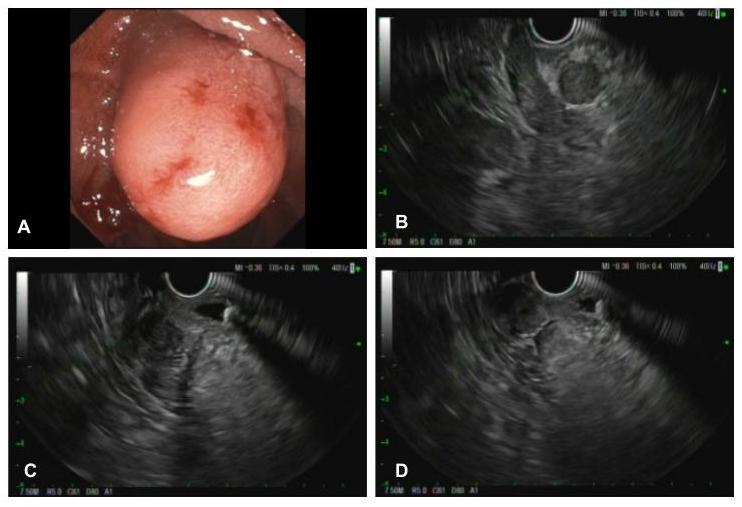
Case Description/Methods: A 58-year-old woman with a history of gastroesophageal reflux disease presented with epigastric pain and reflux refractory to omeprazole and famotidine. Past medical history was notable for remote cholecystectomy. Preliminary esophagogastroduodenoscopy (EGD) found a single 1.5cm subepithelial smooth nodule at the AV with an otherwise normal appearing duodenum. Of note, she had not experienced any jaundice. There were no recent liver enzymes available for review. She was referred for further evaluation with EGD and endoscopic ultrasound. Subsequent EGD visualized a small hiatal hernia and found the subepithelial mass lesion at the AV to be ulcerated. Multiple superficial biopsies of the major papilla were collected for pathology. EUS demonstrated a 2cm x 1.5cm hyperechoic, homogenous, and round mass in the AV. The common bile duct (CBD) was dilated, measuring up to 9mm and multiple stones were visualized in the CBD. Hyperechoic strands were also seen across the entire pancreas. Fine needle biopsy of the ampullary mass revealed a well differentiated neuroendocrine neoplasm with nests of tumor cells with plasmacytoid morphology. She was seen in surgical oncology for staging with plan for pancreaticoduodenectomy with gastrojejunal tube placement.
Discussion: AV NETs are a rare diagnosis, accounting for an estimated < 1% of gastrointestinal NETs and < 2% of ampullary malignancies. Clinical presentation and tumor behavior is diverse, however common symptoms include abdominal pain, jaundice, and weight loss. Primary AV NETs are frequently too small to achieve high MRI sensitivity, making EUS a frontline diagnostic modality. Incidence of AV NETs has increased in recent years owing to improved diagnostic capabilities of newer endoscopic instruments. While there is no standard therapy for AV NETs, larger tumors are typically resected by pancreaticoduodenectomy followed by lymphadenectomy for lymph node involvement which occurs in almost half of AV NETs. However, the rate of postoperative complications such as leaks, bleeding and sepsis is high. Recent reports have suggested endoscopic papillectomy as a lower risk alternative but remains controversial and less suitable for tumors >1cm, which carry higher risk of lymph node metastasis.
Disclosures:
Erika A. Tsuchiyose, BA1, Michael Talanian, MD2, Erik Holzwanger, MD2. P4541 - Neuroendocrine Tumor of the Ampulla of Vater: A Rare Cause of Biliary Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Erika A. Tsuchiyose, BA1, Michael Talanian, MD2, Erik Holzwanger, MD2
1Tufts University School of Medicine, Boston, MA; 2Tufts Medical Center, Boston, MA
Introduction: Neuroendocrine tumor (NET) of the ampulla of Vater (AV) is an exceedingly rare cause of biliary obstruction. We present an unusual case of a subepithelial ampullary NET leading to biliary obstruction diagnosed with endoscopic ultrasound (EUS).
Case Description/Methods: A 58-year-old woman with a history of gastroesophageal reflux disease presented with epigastric pain and reflux refractory to omeprazole and famotidine. Past medical history was notable for remote cholecystectomy. Preliminary esophagogastroduodenoscopy (EGD) found a single 1.5cm subepithelial smooth nodule at the AV with an otherwise normal appearing duodenum. Of note, she had not experienced any jaundice. There were no recent liver enzymes available for review. She was referred for further evaluation with EGD and endoscopic ultrasound. Subsequent EGD visualized a small hiatal hernia and found the subepithelial mass lesion at the AV to be ulcerated. Multiple superficial biopsies of the major papilla were collected for pathology. EUS demonstrated a 2cm x 1.5cm hyperechoic, homogenous, and round mass in the AV. The common bile duct (CBD) was dilated, measuring up to 9mm and multiple stones were visualized in the CBD. Hyperechoic strands were also seen across the entire pancreas. Fine needle biopsy of the ampullary mass revealed a well differentiated neuroendocrine neoplasm with nests of tumor cells with plasmacytoid morphology. She was seen in surgical oncology for staging with plan for pancreaticoduodenectomy with gastrojejunal tube placement.
Discussion: AV NETs are a rare diagnosis, accounting for an estimated < 1% of gastrointestinal NETs and < 2% of ampullary malignancies. Clinical presentation and tumor behavior is diverse, however common symptoms include abdominal pain, jaundice, and weight loss. Primary AV NETs are frequently too small to achieve high MRI sensitivity, making EUS a frontline diagnostic modality. Incidence of AV NETs has increased in recent years owing to improved diagnostic capabilities of newer endoscopic instruments. While there is no standard therapy for AV NETs, larger tumors are typically resected by pancreaticoduodenectomy followed by lymphadenectomy for lymph node involvement which occurs in almost half of AV NETs. However, the rate of postoperative complications such as leaks, bleeding and sepsis is high. Recent reports have suggested endoscopic papillectomy as a lower risk alternative but remains controversial and less suitable for tumors >1cm, which carry higher risk of lymph node metastasis.
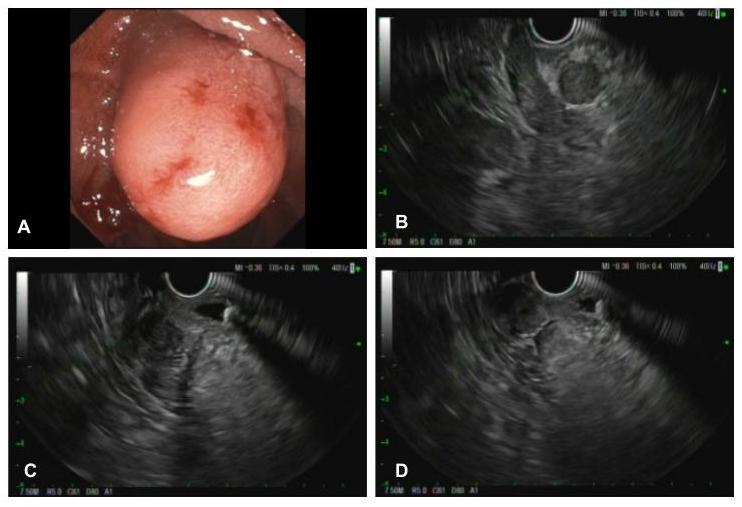
Figure: Figure 1. A) Ulcerated subepithelial mass in the second portion of duodenum, originating from the area of the major papilla B) EUS showing image of the subepithelial ampullary mass C & D) EUS demonstrating circumferential ampullary mass with dilation of the bile duct and hyperechoic biliary stone with associated image shadowing.
Disclosures:
Erika Tsuchiyose indicated no relevant financial relationships.
Michael Talanian indicated no relevant financial relationships.
Erik Holzwanger: Boston Scientific – Consultant.
Erika A. Tsuchiyose, BA1, Michael Talanian, MD2, Erik Holzwanger, MD2. P4541 - Neuroendocrine Tumor of the Ampulla of Vater: A Rare Cause of Biliary Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

