Tuesday Poster Session
Category: Interventional Endoscopy
P4546 - Does Endoscopic Sleeve Gastroplasty Worsen Acid Reflux?
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
William W. King, MD
University of Florida College of Medicine
GAINESVILLE, FL
Presenting Author(s)
William King, MD1, Nathan Northern, MD1, Michael Ladna, MD2, Manuel Amaris, MD1, David Estores, MD1, April Goddard, PA-C1, Bashar Qumseya, MD, MPH1
1University of Florida College of Medicine, Gainesville, FL; 2University of California Davis School of Medicine, Sacramento, CA
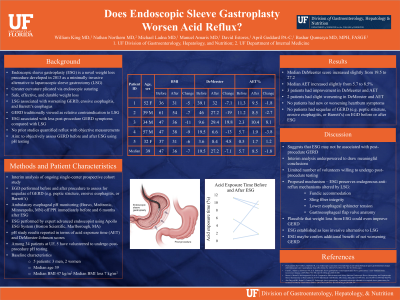
Introduction: Endoscopic sleeve gastroplasty (ESG) is a novel weight loss procedure involving plication of the greater curvature via endoscopic suturing. It has been shown to be safe and effective for achieving durable weight loss. Obesity is a major risk factor for gastroesophageal reflux disease (GERD), which affects up to 30% of the general population. Laparoscopic sleeve gastrectomy (LSG) is associated with worsening GERD, and erosive esophagitis and is now known as a major risk factor for Barrett’s esophagus. ESG, on the other hand, has not been associated with worsening GERD symptoms in a recent multicenter randomized trial. We aimed to objectively assess GERD before and after ESG using pH testing.
Case Description/Methods: This is an interim analysis of an ongoing single center prospective study. Metrics were obtained before and six months after the procedure. We quantified GERD symptoms using the GERD-Q questionnaire and measured acid reflux using wireless pH monitoring (Bravo) or pH and impedance testing.
So far, four patients have had pH testing both before and after ESG. Three patients were male. The median age was 46. The median body mass index (BMI) declined from 47 to 35 in the first six months after the procedure. Among the two who underwent esophagogastroduodenoscopy (EGD) before the procedure, both had normal EGD findings both before and after ESG. The two remaining patients who did not undergo EGD before the procedure did not have any abnormalities on EGD after the procedure.
Median total acid exposure time (AET) trended from 8.5 to 9.0%, and median DeMeester score from 29 to 31. Three patients saw improvement in AET and reported improvement in heartburn symptoms. The fourth patient had slight worsening of AET. He reported ongoing, unchanged heartburn after the procedure.
Discussion: This interim analysis is underpowered but suggests that ESG may not be associated with post-procedure GERD or esophageal dysmotility. One proposed mechanism is that ESG preserves endogenous anti-reflux mechanisms that can be altered by LSG, including fundic accommodation, sling fiber integrity, lower esophageal sphincter tension, and gastroesophageal flap valve anatomy. ESG may thus offer several advantages over traditional LSG as a less invasive procedure preserving esophageal motility and anti-reflux barrier anatomy with lower risk of post-procedure GERD. Ongoing research will further explore this hypothesis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
William King, MD1, Nathan Northern, MD1, Michael Ladna, MD2, Manuel Amaris, MD1, David Estores, MD1, April Goddard, PA-C1, Bashar Qumseya, MD, MPH1. P4546 - Does Endoscopic Sleeve Gastroplasty Worsen Acid Reflux?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Florida College of Medicine, Gainesville, FL; 2University of California Davis School of Medicine, Sacramento, CA
Introduction: Endoscopic sleeve gastroplasty (ESG) is a novel weight loss procedure involving plication of the greater curvature via endoscopic suturing. It has been shown to be safe and effective for achieving durable weight loss. Obesity is a major risk factor for gastroesophageal reflux disease (GERD), which affects up to 30% of the general population. Laparoscopic sleeve gastrectomy (LSG) is associated with worsening GERD, and erosive esophagitis and is now known as a major risk factor for Barrett’s esophagus. ESG, on the other hand, has not been associated with worsening GERD symptoms in a recent multicenter randomized trial. We aimed to objectively assess GERD before and after ESG using pH testing.
Case Description/Methods: This is an interim analysis of an ongoing single center prospective study. Metrics were obtained before and six months after the procedure. We quantified GERD symptoms using the GERD-Q questionnaire and measured acid reflux using wireless pH monitoring (Bravo) or pH and impedance testing.
So far, four patients have had pH testing both before and after ESG. Three patients were male. The median age was 46. The median body mass index (BMI) declined from 47 to 35 in the first six months after the procedure. Among the two who underwent esophagogastroduodenoscopy (EGD) before the procedure, both had normal EGD findings both before and after ESG. The two remaining patients who did not undergo EGD before the procedure did not have any abnormalities on EGD after the procedure.
Median total acid exposure time (AET) trended from 8.5 to 9.0%, and median DeMeester score from 29 to 31. Three patients saw improvement in AET and reported improvement in heartburn symptoms. The fourth patient had slight worsening of AET. He reported ongoing, unchanged heartburn after the procedure.
Discussion: This interim analysis is underpowered but suggests that ESG may not be associated with post-procedure GERD or esophageal dysmotility. One proposed mechanism is that ESG preserves endogenous anti-reflux mechanisms that can be altered by LSG, including fundic accommodation, sling fiber integrity, lower esophageal sphincter tension, and gastroesophageal flap valve anatomy. ESG may thus offer several advantages over traditional LSG as a less invasive procedure preserving esophageal motility and anti-reflux barrier anatomy with lower risk of post-procedure GERD. Ongoing research will further explore this hypothesis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
William King indicated no relevant financial relationships.
Nathan Northern indicated no relevant financial relationships.
Michael Ladna indicated no relevant financial relationships.
Manuel Amaris indicated no relevant financial relationships.
David Estores indicated no relevant financial relationships.
April Goddard indicated no relevant financial relationships.
Bashar Qumseya indicated no relevant financial relationships.
William King, MD1, Nathan Northern, MD1, Michael Ladna, MD2, Manuel Amaris, MD1, David Estores, MD1, April Goddard, PA-C1, Bashar Qumseya, MD, MPH1. P4546 - Does Endoscopic Sleeve Gastroplasty Worsen Acid Reflux?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
