Tuesday Poster Session
Category: Interventional Endoscopy
P4556 - A Case of a Malignant Ampullary Ulceration
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Peter A. Iskander, MD
The Wright Center for Graduate Medical Education
Dunmore, PA
Presenting Author(s)
Peter A. Iskander, MD1, Hany Eskarous, MD1, Mina Daniel, MD2, Khadijah Sajid, MD3, Kanith Farah, MD4, Aman Ali, MD5
1The Wright Center for Graduate Medical Education, Dunmore, PA; 2Memorial Hermann Healthcare System, Cypress, TX; 3The Wright Center for Graduate Medical Education, Scranton, PA; 4West Virginia University, Morgantown, WV; 5Wilkes-Barre General Hospital, Edwardsville, PA
Introduction: Ampullary carcinomas (AC) are rare tumors, accounting for ~0.2% of gastrointestinal cancers, associated with the Ampulla of Vater. Given their location, AC starts presenting earlier than most malignancies due to symptoms of biliary obstruction. ACs generally have a better prognosis, secondary to earlier detection, with a 5-year survival rate of 45% in patients undergoing resection.
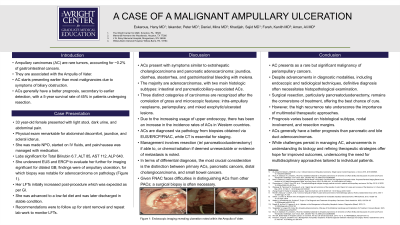
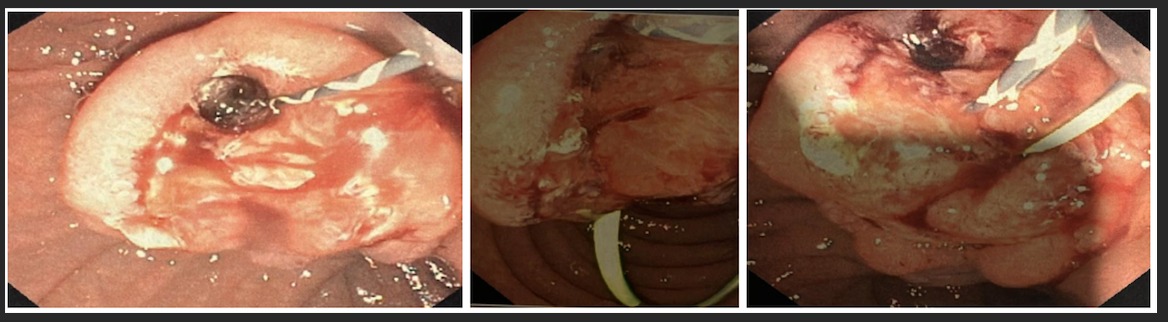
Case Description/Methods: 33 year-old female presented with light stool, dark urine, and abdominal pain. Physical exam remarkable for abdominal discomfort, jaundice, and scleral icterus. She was made NPO, started on IV fluids, and pain/nausea was managed with medication. Labs significant for Total Bilirubin 6.7, ALT 85, AST 112, ALP 640. She underwent EUS and ERCP to evaluate her further for imaging significant for dilated GB; findings were of ampullary ulceration, for which biopsy was notable for adenocarcinoma on pathology (Figure 1). Her LFTs initially increased post-procedure which was expected as per GI. She was advanced to a low-fat diet and was later discharged in stable condition. Recommendations were to follow up for stent removal and repeat lab work to monitor LFTs.
Discussion: ACs present with symptoms similar to extrahepatic cholangiocarcinoma and pancreatic adenocarcinoma: jaundice, diarrhea, steatorrhea, and gastrointestinal bleeding with melena. The majority are adenocarcinomas, with two main histologic subtypes: intestinal and pancreaticobiliary-associated ACs. Three distinct categories of carcinomas are recognized after the correlation of gross and microscopic features: intra-ampullary neoplasms, periampullary, and mixed exophytic/ulcerated lesions. Due to the increasing usage of upper endoscopy, there has been an increase in the incidence rates of ACs in Western countries. ACs are diagnosed via pathology from biopsies obtained via EUS/ERCP/FNAC, while CT is essential for staging. Management involves resection (ie/ pancreaticoduodenectomy) if able to, or chemo/radiation if deemed unresectable or evidence of metastasis is noted. In terms of differential diagnosis, the most crucial consideration is the distinction between primary ACs, pancreatic cancers, distal cholangiocarcinoma, and small bowel cancers. Given FNAC faces difficulties in distinguishing ACs from other PACs; a surgical biopsy is often necessary.
Disclosures:
Peter A. Iskander, MD1, Hany Eskarous, MD1, Mina Daniel, MD2, Khadijah Sajid, MD3, Kanith Farah, MD4, Aman Ali, MD5. P4556 - A Case of a Malignant Ampullary Ulceration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Wright Center for Graduate Medical Education, Dunmore, PA; 2Memorial Hermann Healthcare System, Cypress, TX; 3The Wright Center for Graduate Medical Education, Scranton, PA; 4West Virginia University, Morgantown, WV; 5Wilkes-Barre General Hospital, Edwardsville, PA
Introduction: Ampullary carcinomas (AC) are rare tumors, accounting for ~0.2% of gastrointestinal cancers, associated with the Ampulla of Vater. Given their location, AC starts presenting earlier than most malignancies due to symptoms of biliary obstruction. ACs generally have a better prognosis, secondary to earlier detection, with a 5-year survival rate of 45% in patients undergoing resection.
Case Description/Methods: 33 year-old female presented with light stool, dark urine, and abdominal pain. Physical exam remarkable for abdominal discomfort, jaundice, and scleral icterus. She was made NPO, started on IV fluids, and pain/nausea was managed with medication. Labs significant for Total Bilirubin 6.7, ALT 85, AST 112, ALP 640. She underwent EUS and ERCP to evaluate her further for imaging significant for dilated GB; findings were of ampullary ulceration, for which biopsy was notable for adenocarcinoma on pathology (Figure 1). Her LFTs initially increased post-procedure which was expected as per GI. She was advanced to a low-fat diet and was later discharged in stable condition. Recommendations were to follow up for stent removal and repeat lab work to monitor LFTs.
Discussion: ACs present with symptoms similar to extrahepatic cholangiocarcinoma and pancreatic adenocarcinoma: jaundice, diarrhea, steatorrhea, and gastrointestinal bleeding with melena. The majority are adenocarcinomas, with two main histologic subtypes: intestinal and pancreaticobiliary-associated ACs. Three distinct categories of carcinomas are recognized after the correlation of gross and microscopic features: intra-ampullary neoplasms, periampullary, and mixed exophytic/ulcerated lesions. Due to the increasing usage of upper endoscopy, there has been an increase in the incidence rates of ACs in Western countries. ACs are diagnosed via pathology from biopsies obtained via EUS/ERCP/FNAC, while CT is essential for staging. Management involves resection (ie/ pancreaticoduodenectomy) if able to, or chemo/radiation if deemed unresectable or evidence of metastasis is noted. In terms of differential diagnosis, the most crucial consideration is the distinction between primary ACs, pancreatic cancers, distal cholangiocarcinoma, and small bowel cancers. Given FNAC faces difficulties in distinguishing ACs from other PACs; a surgical biopsy is often necessary.
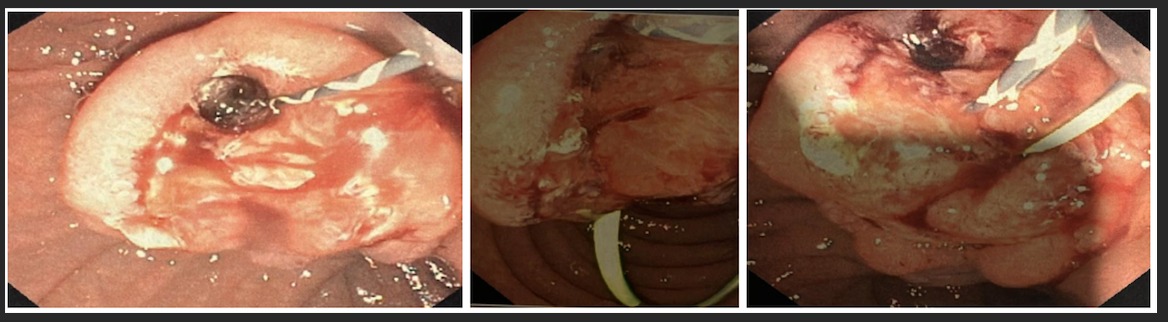
Figure: Figure 1: Endoscopic imaging revealing ulceration noted within the Ampulla of Vater.
Disclosures:
Peter Iskander indicated no relevant financial relationships.
Hany Eskarous indicated no relevant financial relationships.
Mina Daniel indicated no relevant financial relationships.
Khadijah Sajid indicated no relevant financial relationships.
Kanith Farah indicated no relevant financial relationships.
Aman Ali indicated no relevant financial relationships.
Peter A. Iskander, MD1, Hany Eskarous, MD1, Mina Daniel, MD2, Khadijah Sajid, MD3, Kanith Farah, MD4, Aman Ali, MD5. P4556 - A Case of a Malignant Ampullary Ulceration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
