Tuesday Poster Session
Category: Interventional Endoscopy
P4558 - Hidden Connections: A Case of Gastrocolic Fistula From Gastrojejunostomy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SB
Shoujit Banerjee, MD
University of California Irvine
Orange, CA
Presenting Author(s)
Shoujit Banerjee, MD1, Bryant Le, MD1, Marie Balfour, MD2, Trevor McCracken, MD1, Joshua Kwon, MD1, Peter H. Nguyen, MD2, Jason Samarasena, MD2, John G. Lee, MD2, Frances Dang, MD2
1University of California Irvine, Orange, CA; 2University of California, Irvine, Orange, CA
Introduction: Gastrocolic fistulas are rare connections that form between the stomach and colon. Patients may present with weight loss, diarrhea, and vomiting. The following is a unique case of persistent diarrhea ultimately found to be secondary to gastrocolic fistula caused by a migrated lumen apposing metal stent (LAMS).
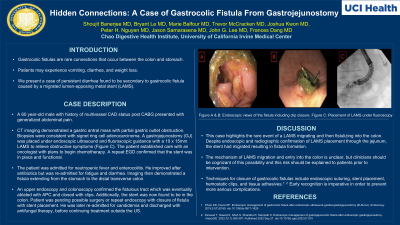
Case Description/Methods: A 60 year-old man with multivessel CAD status post CABG presented for abdominal pain. CT imaging revealed a gastric antral mass with partial gastric outlet obstruction with biopsies showing Signet ring cell adenocarcinoma. A gastrojejunostomy (GJ) was placed under endoscopic ultrasound and fluoroscopic guidance with a 10 x 15mm LAMS to relieve obstructive symptoms (Image C). He established care with an oncologist with a plan to start chemotherapy. During a repeat EGD, the stent was confirmed in place and functional. Soon after chemotherapy started, he was admitted for neutropenic fever and enterocolitis, with enteropathogenic E. Coli (EPEC) growing in stool studies. The patient improved after antibiotic treatment but was re-admitted for fatigue and recurrent diarrhea; repeat CT imaging now showed presence of a fistula extending from the stomach to the distal transverse colon. An upper endoscopy and colonoscopy confirmed the fistulous tract, which was ablated with APC and closed with clips. Patient currently awaits definitive surgical repair of the fistula.
Discussion: Endoscopic Gastrojejunostomy with LAMS is a tremendous advance in medicine for the management of gastroduodenal outlet obstruction in oncologic patients. In this case, we report a rare case of a LAMS migrating and then fistulizing into the colon. There have been several instances of LAMS being inadvertently placed into the colon at the time of an attempted gastrojejunostomy. In this case, we were certain that the LAMS was originally placed in the jejunum based on radiographic and direct endoscopic examination through the stent. The mechanism of LAMS migration and entry into the colon are unclear but warrant consideration. The possibility of a gastrocolic fistula should be mentioned to patients during consent as a risk when these procedures are being performed. Definitive management will likely require endoscopic or surgical intervention and early recognition is key to prevent more serious complications.

Disclosures:
Shoujit Banerjee, MD1, Bryant Le, MD1, Marie Balfour, MD2, Trevor McCracken, MD1, Joshua Kwon, MD1, Peter H. Nguyen, MD2, Jason Samarasena, MD2, John G. Lee, MD2, Frances Dang, MD2. P4558 - Hidden Connections: A Case of Gastrocolic Fistula From Gastrojejunostomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California Irvine, Orange, CA; 2University of California, Irvine, Orange, CA
Introduction: Gastrocolic fistulas are rare connections that form between the stomach and colon. Patients may present with weight loss, diarrhea, and vomiting. The following is a unique case of persistent diarrhea ultimately found to be secondary to gastrocolic fistula caused by a migrated lumen apposing metal stent (LAMS).
Case Description/Methods: A 60 year-old man with multivessel CAD status post CABG presented for abdominal pain. CT imaging revealed a gastric antral mass with partial gastric outlet obstruction with biopsies showing Signet ring cell adenocarcinoma. A gastrojejunostomy (GJ) was placed under endoscopic ultrasound and fluoroscopic guidance with a 10 x 15mm LAMS to relieve obstructive symptoms (Image C). He established care with an oncologist with a plan to start chemotherapy. During a repeat EGD, the stent was confirmed in place and functional. Soon after chemotherapy started, he was admitted for neutropenic fever and enterocolitis, with enteropathogenic E. Coli (EPEC) growing in stool studies. The patient improved after antibiotic treatment but was re-admitted for fatigue and recurrent diarrhea; repeat CT imaging now showed presence of a fistula extending from the stomach to the distal transverse colon. An upper endoscopy and colonoscopy confirmed the fistulous tract, which was ablated with APC and closed with clips. Patient currently awaits definitive surgical repair of the fistula.
Discussion: Endoscopic Gastrojejunostomy with LAMS is a tremendous advance in medicine for the management of gastroduodenal outlet obstruction in oncologic patients. In this case, we report a rare case of a LAMS migrating and then fistulizing into the colon. There have been several instances of LAMS being inadvertently placed into the colon at the time of an attempted gastrojejunostomy. In this case, we were certain that the LAMS was originally placed in the jejunum based on radiographic and direct endoscopic examination through the stent. The mechanism of LAMS migration and entry into the colon are unclear but warrant consideration. The possibility of a gastrocolic fistula should be mentioned to patients during consent as a risk when these procedures are being performed. Definitive management will likely require endoscopic or surgical intervention and early recognition is key to prevent more serious complications.

Figure: Figure A & B: Endoscopic views of the fistula including clip closure. Figure C: Gastrojejunostomy placement
Disclosures:
Shoujit Banerjee indicated no relevant financial relationships.
Bryant Le indicated no relevant financial relationships.
Marie Balfour indicated no relevant financial relationships.
Trevor McCracken indicated no relevant financial relationships.
Joshua Kwon indicated no relevant financial relationships.
Peter Nguyen indicated no relevant financial relationships.
Jason Samarasena: Cook Medical – Consultant. Medtronic – Advisory Committee/Board Member, Consultant. Neptune Medical – Advisory Committee/Board Member, Consultant. Olympus – Advisory Committee/Board Member, Consultant. Ovesco – Advisory Committee/Board Member, Consultant, Speakers Bureau. SatisfAI – Stock-privately held company. Steris – Advisory Committee/Board Member.
John Lee indicated no relevant financial relationships.
Frances Dang indicated no relevant financial relationships.
Shoujit Banerjee, MD1, Bryant Le, MD1, Marie Balfour, MD2, Trevor McCracken, MD1, Joshua Kwon, MD1, Peter H. Nguyen, MD2, Jason Samarasena, MD2, John G. Lee, MD2, Frances Dang, MD2. P4558 - Hidden Connections: A Case of Gastrocolic Fistula From Gastrojejunostomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
