Tuesday Poster Session
Category: Interventional Endoscopy
P4561 - Successful Endoscopic Management of Near-Fatal Boerhaave's Syndrome in High-Risk Non-Operative Patient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

David L. Hobby, MD
Atrium Health/Navicent
Valdosta, GA
Presenting Author(s)
David L. Hobby, MD1, Roxana Coman, MD, PhD2, James Foster, MD2, Laura Reed, MD2, Elizabeth L. Lowry, PA2
1Atrium Health/Navicent, Valdosta, GA; 2Atrium Health/Navicent, Macon, GA
Introduction: Severe Boerhaave’s syndrome with complete detachment of the esophagus from cardia was ultimately managed with endoscopic intervention using fully covered self-expandable metal esophageal stent as patient was deemed non-operative candidate.
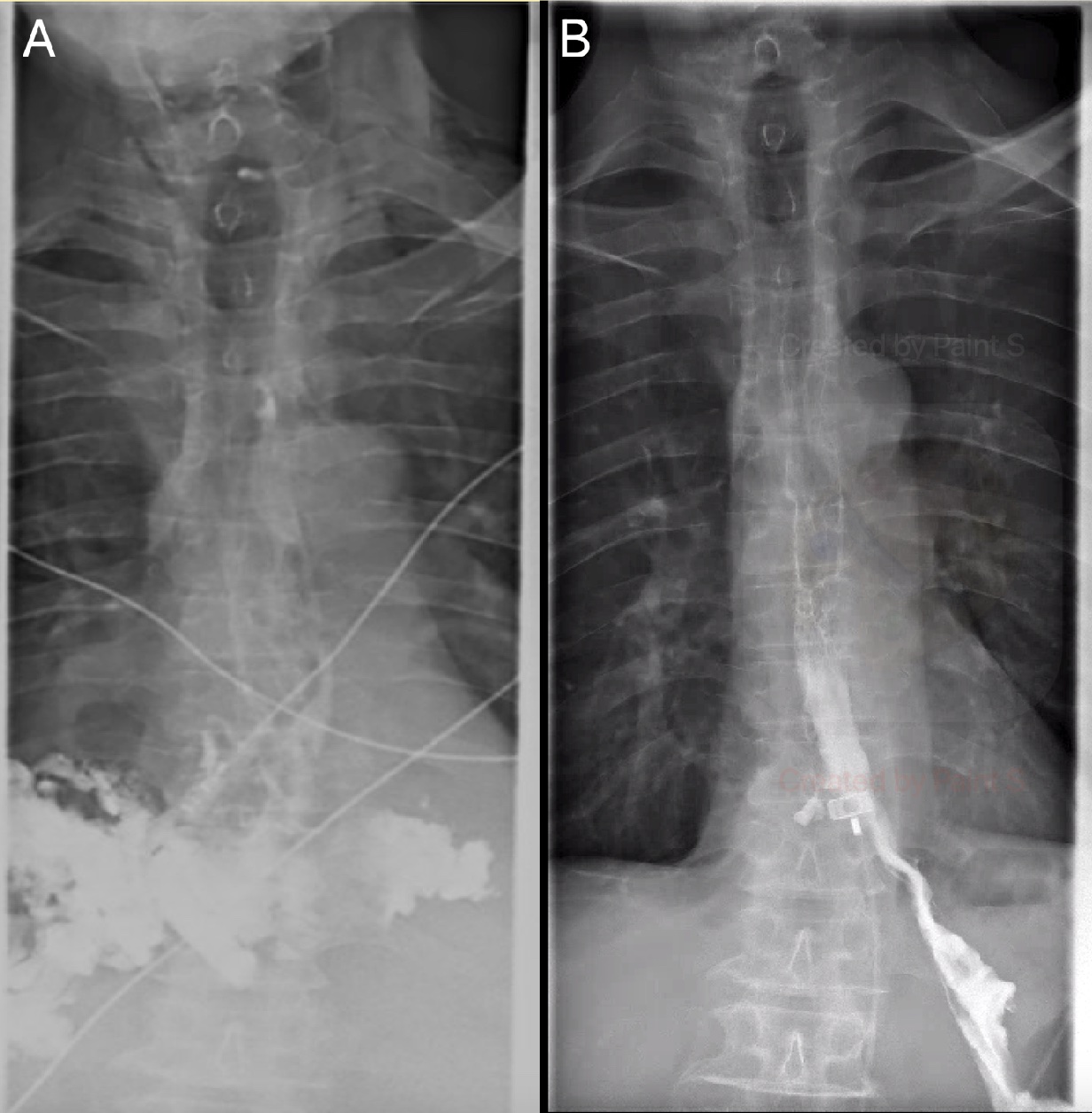
Case Description/Methods: A 58-year-old male presented with septic shock with evidence of esophageal perforation symptomatic for three days duration. CT chest noted extensive posterior and superior pneumomediastinum. CT esophagram confirmed a complete distal esophageal transection with significant extraluminal extravasation of contrast with no progression to stomach (Figure 1a). Patient underwent right thoracotomy with decortication, mediastinal drainage, and left tube placement noting copious necrotic output growing E. aerogenes and C. albicans. Patient was deemed too unstable for surgical intervention due to duration and extent of perforation and clinical status. Endoscopic evaluation noted 30 mm long circumferential esophageal tear in the lower third of the esophagus with complete transection of the esophagus. A 23 mm x 152 mm fully covered stent (Wallflex, Boston) was placed anchored by two hemostatic clips (Sureclip, Microtech). Due to large luminal defect as well as intrathoracic negative pressure, the distal end of the esophageal stent was displaced into the mediastinal space. To secure optimal stent position, the proximal end of the stent was anchored to the esophageal wall using an over-the-scope clip (Padlock, Steris). Serial imaging confirmed successful placement without migration, and the patient was discharged. Patient returned in 8 weeks for endoscopic stent removal. First Attempt to remove the clip anchoring the stent using flexible endoscope was unsuccessful. On the second attempt, in a staged endoscopic approach, the OVES clip was excised using a rigid endoscope, and the stent was removed with the flexible endoscope. Examination of the esophagus showed reconstitution of the esophageal lumen with granulation tissue with complete absence of mucosal lining. At 1-month follow-up, the patient was asymptomatic, tolerating full diet. The esophagram showed only mild distal esophageal stricture, without evidence of extraluminal leak (Figure 1b).
Discussion: This case illustrates how appropriate endoscopic management combined with medical management in a patient with near-fatal, non-operative Boerhaave's syndrome allowed native granulation tissue to seal around the esophageal stent to reshape the distal esophageal lumen in the absence of mucosal lining.
Disclosures:
David L. Hobby, MD1, Roxana Coman, MD, PhD2, James Foster, MD2, Laura Reed, MD2, Elizabeth L. Lowry, PA2. P4561 - Successful Endoscopic Management of Near-Fatal Boerhaave's Syndrome in High-Risk Non-Operative Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Atrium Health/Navicent, Valdosta, GA; 2Atrium Health/Navicent, Macon, GA
Introduction: Severe Boerhaave’s syndrome with complete detachment of the esophagus from cardia was ultimately managed with endoscopic intervention using fully covered self-expandable metal esophageal stent as patient was deemed non-operative candidate.
Case Description/Methods: A 58-year-old male presented with septic shock with evidence of esophageal perforation symptomatic for three days duration. CT chest noted extensive posterior and superior pneumomediastinum. CT esophagram confirmed a complete distal esophageal transection with significant extraluminal extravasation of contrast with no progression to stomach (Figure 1a). Patient underwent right thoracotomy with decortication, mediastinal drainage, and left tube placement noting copious necrotic output growing E. aerogenes and C. albicans. Patient was deemed too unstable for surgical intervention due to duration and extent of perforation and clinical status. Endoscopic evaluation noted 30 mm long circumferential esophageal tear in the lower third of the esophagus with complete transection of the esophagus. A 23 mm x 152 mm fully covered stent (Wallflex, Boston) was placed anchored by two hemostatic clips (Sureclip, Microtech). Due to large luminal defect as well as intrathoracic negative pressure, the distal end of the esophageal stent was displaced into the mediastinal space. To secure optimal stent position, the proximal end of the stent was anchored to the esophageal wall using an over-the-scope clip (Padlock, Steris). Serial imaging confirmed successful placement without migration, and the patient was discharged. Patient returned in 8 weeks for endoscopic stent removal. First Attempt to remove the clip anchoring the stent using flexible endoscope was unsuccessful. On the second attempt, in a staged endoscopic approach, the OVES clip was excised using a rigid endoscope, and the stent was removed with the flexible endoscope. Examination of the esophagus showed reconstitution of the esophageal lumen with granulation tissue with complete absence of mucosal lining. At 1-month follow-up, the patient was asymptomatic, tolerating full diet. The esophagram showed only mild distal esophageal stricture, without evidence of extraluminal leak (Figure 1b).
Discussion: This case illustrates how appropriate endoscopic management combined with medical management in a patient with near-fatal, non-operative Boerhaave's syndrome allowed native granulation tissue to seal around the esophageal stent to reshape the distal esophageal lumen in the absence of mucosal lining.
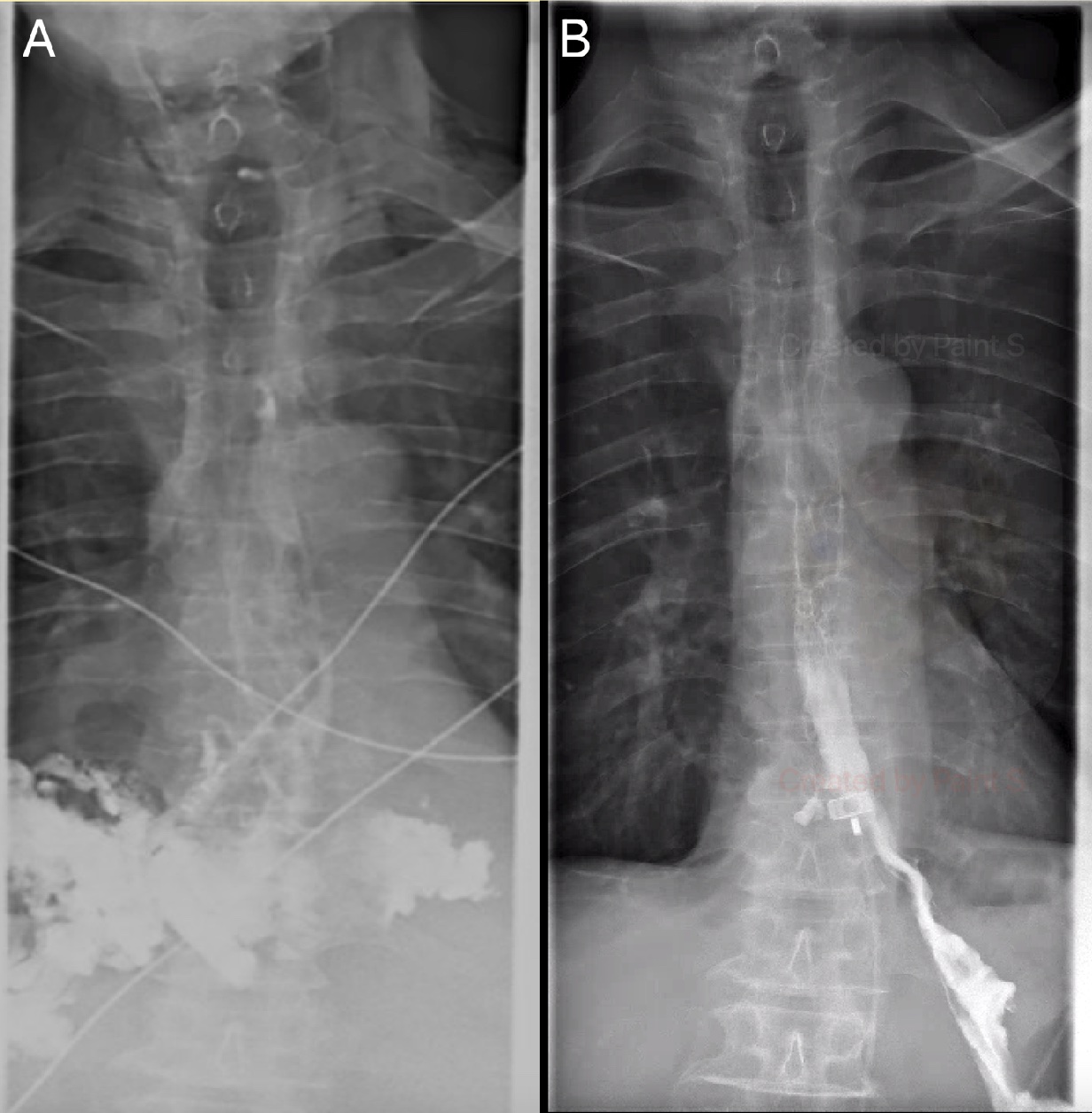
Figure: Figure 1A notes complete extravasation of contrast consistent with perforation. Figure 1B demonstrates the newly formed granulation tissue creating a seal around the stent following stent removal.
Disclosures:
David Hobby indicated no relevant financial relationships.
Roxana Coman indicated no relevant financial relationships.
James Foster indicated no relevant financial relationships.
Laura Reed indicated no relevant financial relationships.
Elizabeth Lowry indicated no relevant financial relationships.
David L. Hobby, MD1, Roxana Coman, MD, PhD2, James Foster, MD2, Laura Reed, MD2, Elizabeth L. Lowry, PA2. P4561 - Successful Endoscopic Management of Near-Fatal Boerhaave's Syndrome in High-Risk Non-Operative Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

