Tuesday Poster Session
Category: Liver
P4589 - Assessment of Genetic Variants and Ancestry in Lean and Non-Lean MASLD Patients in a Latin American Cohort
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Amir Sultan Seid, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Amir Sultan Seid, MD1, Jhon Prieto, MD2, Domingo Bladerramo, MD3, Javier Diaz Ferrer, MD4, Angelo Z. Mattos, MD, PhD5, Marco Arrese, MD6, Enrique Carrera, MD7, Andre Boonstra, PhD8, Jose Debes, MD, PhD1
1University of Minnesota, Minneapolis, MN; 2Centro de Enfermedades Hepaticas y Digestives, Bogota, Distrito Capital de Bogota, Colombia; 3Hospital Privado Universitario de Cordoba, Cordoba, Cordoba, Argentina; 4Universidad San Martin de Porres, Lima, Lima, Peru; 5Federal University of Health Sciences of Porto Alegre, Porto Alegre, Rio Grande do Sul, Brazil; 6Pontificia Universidad Católica de Chile, Santiago, Region Metropolitana, Chile; 7Universidad San Francisco de Quito, Quito, Pichincha, Ecuador; 8Erasmus University Medical Center, Rotterdam, Zuid-Holland, Netherlands
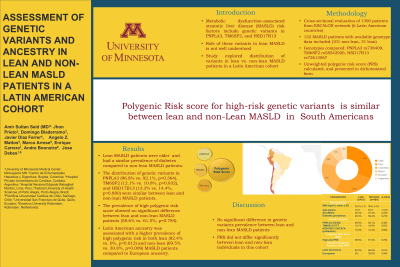
Introduction: Risk factors for Metabolic dysfunction-associated steatotic liver disease (MASLD) include genetic variants in PNPLA3 TM6SF2 and HSD17B13. The role of these variants in lean MASLD is not well understood. We explored the distribution of these variants in lean versus non-lean MASLD patients in a Latin American cohort.
Methods: We cross-sectionally evaluated a total of 1300 patients from the ESCALON network, which includes 6 countries across Latin America. Among these, 132 patients with MASLD (101 non-lean, 31 lean) had available genotype data and were included in this analysis. Ancestry was self-reported as Latin American, European, or other. Lean MASLD was defined as MASLD with a BMI < 25 kg/m². Genotypes for PNPLA3 rs738409 (CG/GG vs. CC), TM6SF2 rs58542926 (CT/TT vs. CC), and HSD17B13 rs72613567 (TA/TATA vs. TT/T) were compared between groups. A simple, unweighted polygenic risk score (PRS) combining the three variants was calculated by summing all risk alleles (PNPLA3 G, TM6SF2 T, and HSD17B13 T) for each individual and categorized as low or high. Pearson chi-square and Fisher's exact tests used for analysis.
Results: 31 lean (BMI 23.0±1.6 kg/m2) and 101 non-lean (BMI 30.6±4.5 kg/m2) patients from Argentina (4.5%), Brazil (8.3%), Chile (31.1%), Colombia (22.0%), Ecuador (7.6%), and Peru (26.5%) were analyzed. Lean patients were older (72.0 vs. 67.5 years, p< 0.01) but gender distribution was similar. The prevalence of diabetes was comparable between lean (48.4%) and non-lean (59.4%) groups (p=0.279). PNPLA3 CG/GG prevalence was comparable in lean (96.8%) and non-lean (92.1%) groups (p=0.364). TM6SF2 CT/TT prevalence was similar in lean (12.1%) and non-lean (10.8%) patients (p=0.832), while the protective HSD17B13 TA/TATA variant was present in 13.3% of lean and 14.4% of non-lean patients (p=0.880). The dichotomized PRS showed no difference in high-risk allele prevalence between lean (58.6%) and non-lean (61.5%) patients (p=0.784). In a subgroup analysis based on self-reported ancestry, high PRS was more prevalent in Latin Americans compared to Europeans in both lean (82.4% vs. 0%, p=0.012) and non-lean (69.5% vs. 30.8%, p=0.009) groups.
Discussion: In our cohort the prevalence of PNPLA3, TM6SF2, the HSD17B13 (protective variant), as well as a PRS did not differ significantly between lean and non-lean individuals. The proportion of high-risk PRS was higher in the subgroup of patients of Latin American descent compared to those of European descent in both lean and non-lean groups.
Disclosures:
Amir Sultan Seid, MD1, Jhon Prieto, MD2, Domingo Bladerramo, MD3, Javier Diaz Ferrer, MD4, Angelo Z. Mattos, MD, PhD5, Marco Arrese, MD6, Enrique Carrera, MD7, Andre Boonstra, PhD8, Jose Debes, MD, PhD1. P4589 - Assessment of Genetic Variants and Ancestry in Lean and Non-Lean MASLD Patients in a Latin American Cohort, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2Centro de Enfermedades Hepaticas y Digestives, Bogota, Distrito Capital de Bogota, Colombia; 3Hospital Privado Universitario de Cordoba, Cordoba, Cordoba, Argentina; 4Universidad San Martin de Porres, Lima, Lima, Peru; 5Federal University of Health Sciences of Porto Alegre, Porto Alegre, Rio Grande do Sul, Brazil; 6Pontificia Universidad Católica de Chile, Santiago, Region Metropolitana, Chile; 7Universidad San Francisco de Quito, Quito, Pichincha, Ecuador; 8Erasmus University Medical Center, Rotterdam, Zuid-Holland, Netherlands
Introduction: Risk factors for Metabolic dysfunction-associated steatotic liver disease (MASLD) include genetic variants in PNPLA3 TM6SF2 and HSD17B13. The role of these variants in lean MASLD is not well understood. We explored the distribution of these variants in lean versus non-lean MASLD patients in a Latin American cohort.
Methods: We cross-sectionally evaluated a total of 1300 patients from the ESCALON network, which includes 6 countries across Latin America. Among these, 132 patients with MASLD (101 non-lean, 31 lean) had available genotype data and were included in this analysis. Ancestry was self-reported as Latin American, European, or other. Lean MASLD was defined as MASLD with a BMI < 25 kg/m². Genotypes for PNPLA3 rs738409 (CG/GG vs. CC), TM6SF2 rs58542926 (CT/TT vs. CC), and HSD17B13 rs72613567 (TA/TATA vs. TT/T) were compared between groups. A simple, unweighted polygenic risk score (PRS) combining the three variants was calculated by summing all risk alleles (PNPLA3 G, TM6SF2 T, and HSD17B13 T) for each individual and categorized as low or high. Pearson chi-square and Fisher's exact tests used for analysis.
Results: 31 lean (BMI 23.0±1.6 kg/m2) and 101 non-lean (BMI 30.6±4.5 kg/m2) patients from Argentina (4.5%), Brazil (8.3%), Chile (31.1%), Colombia (22.0%), Ecuador (7.6%), and Peru (26.5%) were analyzed. Lean patients were older (72.0 vs. 67.5 years, p< 0.01) but gender distribution was similar. The prevalence of diabetes was comparable between lean (48.4%) and non-lean (59.4%) groups (p=0.279). PNPLA3 CG/GG prevalence was comparable in lean (96.8%) and non-lean (92.1%) groups (p=0.364). TM6SF2 CT/TT prevalence was similar in lean (12.1%) and non-lean (10.8%) patients (p=0.832), while the protective HSD17B13 TA/TATA variant was present in 13.3% of lean and 14.4% of non-lean patients (p=0.880). The dichotomized PRS showed no difference in high-risk allele prevalence between lean (58.6%) and non-lean (61.5%) patients (p=0.784). In a subgroup analysis based on self-reported ancestry, high PRS was more prevalent in Latin Americans compared to Europeans in both lean (82.4% vs. 0%, p=0.012) and non-lean (69.5% vs. 30.8%, p=0.009) groups.
Discussion: In our cohort the prevalence of PNPLA3, TM6SF2, the HSD17B13 (protective variant), as well as a PRS did not differ significantly between lean and non-lean individuals. The proportion of high-risk PRS was higher in the subgroup of patients of Latin American descent compared to those of European descent in both lean and non-lean groups.
Disclosures:
Amir Sultan Seid indicated no relevant financial relationships.
Jhon Prieto indicated no relevant financial relationships.
Domingo Bladerramo indicated no relevant financial relationships.
Javier Diaz Ferrer indicated no relevant financial relationships.
Angelo Z. Mattos indicated no relevant financial relationships.
Marco Arrese indicated no relevant financial relationships.
Enrique Carrera indicated no relevant financial relationships.
Andre Boonstra indicated no relevant financial relationships.
Jose Debes indicated no relevant financial relationships.
Amir Sultan Seid, MD1, Jhon Prieto, MD2, Domingo Bladerramo, MD3, Javier Diaz Ferrer, MD4, Angelo Z. Mattos, MD, PhD5, Marco Arrese, MD6, Enrique Carrera, MD7, Andre Boonstra, PhD8, Jose Debes, MD, PhD1. P4589 - Assessment of Genetic Variants and Ancestry in Lean and Non-Lean MASLD Patients in a Latin American Cohort, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
