Tuesday Poster Session
Category: Liver
P4592 - Long-Term Risks of Cirrhosis and Hepatocellular Carcinoma Among Treatment Naïve Chronic Hepatitis B Patients by Baseline Hepatitis B Viral Load
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Robert Wong, MD, MS, FACG
Stanford/VA Palo Alto
Palo Alto, CA
Presenting Author(s)
Zeyuan Yang, MS1, Ramsey Cheung, MD2, Janice Jou, MD3, Joseph Lim, MD4, Robert Wong, MD, MS, FACG5
1VA Palo Alto Health Care System, Palo Alto, CA; 2Stanford University School of Medicine, Palo Alto, CA; 3Oregon Health & Science University, Portland, OR; 4Yale University School of Medicine, New Haven, CT; 5Stanford/VA Palo Alto, Palo Alto, CA
Introduction: While antiviral therapy significantly reduces long-term risks of cirrhosis and hepatocellular carcinoma (HCC) among patients with chronic hepatitis B (CHB), major gaps in timely treatment persists. There have been conflicting data on the impact of baseline hepatitis B virus (HBV) DNA on risks of HCC among Asian populations with recent data suggesting higher HCC risk in patients with moderate levels of HBV viral load vs. high levels of HBV DNA. We aim to evaluate the association between baseline HBV DNA and long-term risks of cirrhosis or HCC among a predominantly non-Asian national cohort of Veterans with CHB.
Methods: All adult Veterans with non-cirrhotic treatment-naïve CHB (with baseline HBV DNA > 2,000 IU/mL) were identified from 1/1/2020-3/31/2024 using national longitudinal Veterans Affairs data. Primary outcomes were long-term risks of cirrhosis and HCC (per 100-person-years), stratified by baseline high HBV DNA ( >6.00 log10 IU/mL) or moderate HBV DNA (2,000 – 6.00 log10 IU/mL). Patients were censored at initiation of CHB treatment or death. Propensity score weighting (PSW) was applied to compare long-term outcomes between patients with baseline high HBV DNA vs. moderate HBV DNA. Competing risks cumulative incidence functions and Cox proportional hazards models were utilized.
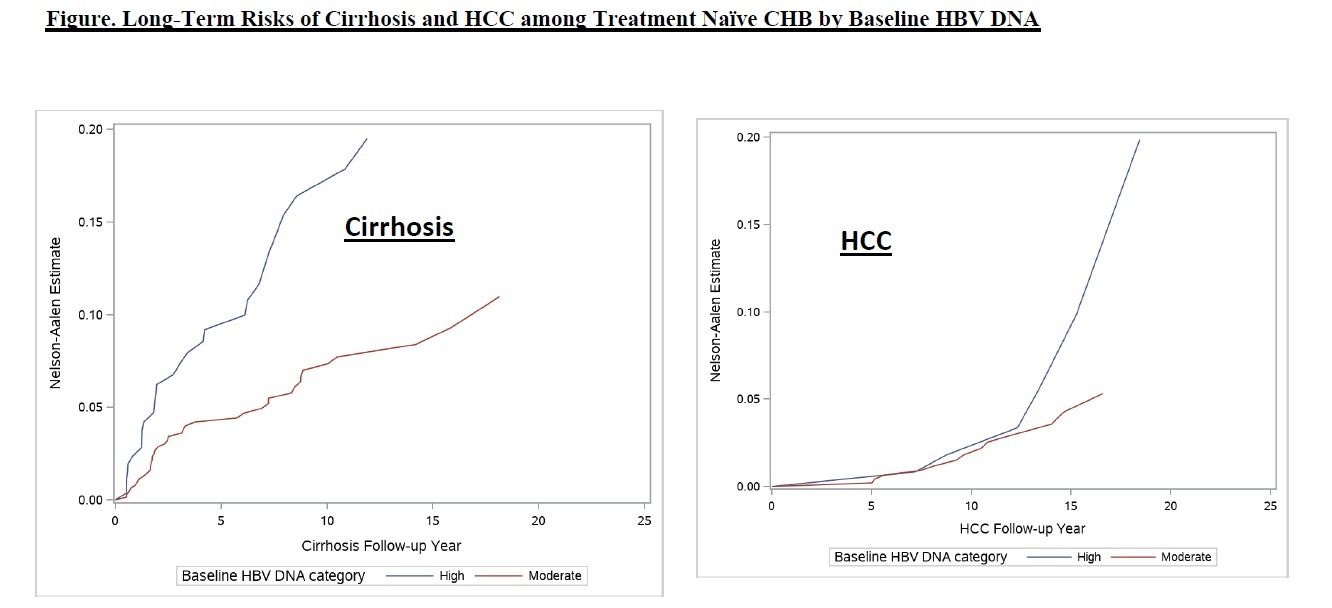
Results: Among 1,198 non-cirrhotic treatment-naïve CHB patients and HBV DNA > 2,000 IU/mL (27.9% HBeAg positive, 90.7% men, 41.7% African Americans, 29.6% non-Hispanic white, 18.2% Asian, mean age 54.7y, 20.8% with diabetes, 12.4% with FIB-4 > 3.25), 67.1% (n=804) had moderate baseline HBV DNA and 32.9% (n=394) had high HBV DNA. Long-term risk of cirrhosis was significantly lower in the moderate baseline HBV DNA group vs. high HBV DNA (0.64 vs. 1.56 per 100-person-years; HR 0.44, 95% CI 0.27-0.71, p< 0.01) (Figure). Risk of HCC was not significantly different in the moderate HBV DNA vs. high HBV DNA groups (0.21 vs. 0.32 per 100-person-years; HR 0.57, 95% CI 0.22-1.51, p=0.26). After PSW, the risk of cirrhosis was no longer significantly different between the moderate vs. high HBV DNA group (HR 0.93, 95% CI 0.68-1.28), and the risk of HCC remained similar between groups (HR 1.02, 95% CI 0.57-1.83).
Discussion: Among a longitudinal national cohort of predominantly non-Asian Veterans with non-cirrhotic treatment naïve CHB, the risk of cirrhosis was higher in the high HBV DNA vs. moderate HBV DNA group. However, after PSW, risks of cirrhosis or HCC were similar by baseline HBV DNA.
Disclosures:
Zeyuan Yang, MS1, Ramsey Cheung, MD2, Janice Jou, MD3, Joseph Lim, MD4, Robert Wong, MD, MS, FACG5. P4592 - Long-Term Risks of Cirrhosis and Hepatocellular Carcinoma Among Treatment Naïve Chronic Hepatitis B Patients by Baseline Hepatitis B Viral Load, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1VA Palo Alto Health Care System, Palo Alto, CA; 2Stanford University School of Medicine, Palo Alto, CA; 3Oregon Health & Science University, Portland, OR; 4Yale University School of Medicine, New Haven, CT; 5Stanford/VA Palo Alto, Palo Alto, CA
Introduction: While antiviral therapy significantly reduces long-term risks of cirrhosis and hepatocellular carcinoma (HCC) among patients with chronic hepatitis B (CHB), major gaps in timely treatment persists. There have been conflicting data on the impact of baseline hepatitis B virus (HBV) DNA on risks of HCC among Asian populations with recent data suggesting higher HCC risk in patients with moderate levels of HBV viral load vs. high levels of HBV DNA. We aim to evaluate the association between baseline HBV DNA and long-term risks of cirrhosis or HCC among a predominantly non-Asian national cohort of Veterans with CHB.
Methods: All adult Veterans with non-cirrhotic treatment-naïve CHB (with baseline HBV DNA > 2,000 IU/mL) were identified from 1/1/2020-3/31/2024 using national longitudinal Veterans Affairs data. Primary outcomes were long-term risks of cirrhosis and HCC (per 100-person-years), stratified by baseline high HBV DNA ( >6.00 log10 IU/mL) or moderate HBV DNA (2,000 – 6.00 log10 IU/mL). Patients were censored at initiation of CHB treatment or death. Propensity score weighting (PSW) was applied to compare long-term outcomes between patients with baseline high HBV DNA vs. moderate HBV DNA. Competing risks cumulative incidence functions and Cox proportional hazards models were utilized.
Results: Among 1,198 non-cirrhotic treatment-naïve CHB patients and HBV DNA > 2,000 IU/mL (27.9% HBeAg positive, 90.7% men, 41.7% African Americans, 29.6% non-Hispanic white, 18.2% Asian, mean age 54.7y, 20.8% with diabetes, 12.4% with FIB-4 > 3.25), 67.1% (n=804) had moderate baseline HBV DNA and 32.9% (n=394) had high HBV DNA. Long-term risk of cirrhosis was significantly lower in the moderate baseline HBV DNA group vs. high HBV DNA (0.64 vs. 1.56 per 100-person-years; HR 0.44, 95% CI 0.27-0.71, p< 0.01) (Figure). Risk of HCC was not significantly different in the moderate HBV DNA vs. high HBV DNA groups (0.21 vs. 0.32 per 100-person-years; HR 0.57, 95% CI 0.22-1.51, p=0.26). After PSW, the risk of cirrhosis was no longer significantly different between the moderate vs. high HBV DNA group (HR 0.93, 95% CI 0.68-1.28), and the risk of HCC remained similar between groups (HR 1.02, 95% CI 0.57-1.83).
Discussion: Among a longitudinal national cohort of predominantly non-Asian Veterans with non-cirrhotic treatment naïve CHB, the risk of cirrhosis was higher in the high HBV DNA vs. moderate HBV DNA group. However, after PSW, risks of cirrhosis or HCC were similar by baseline HBV DNA.
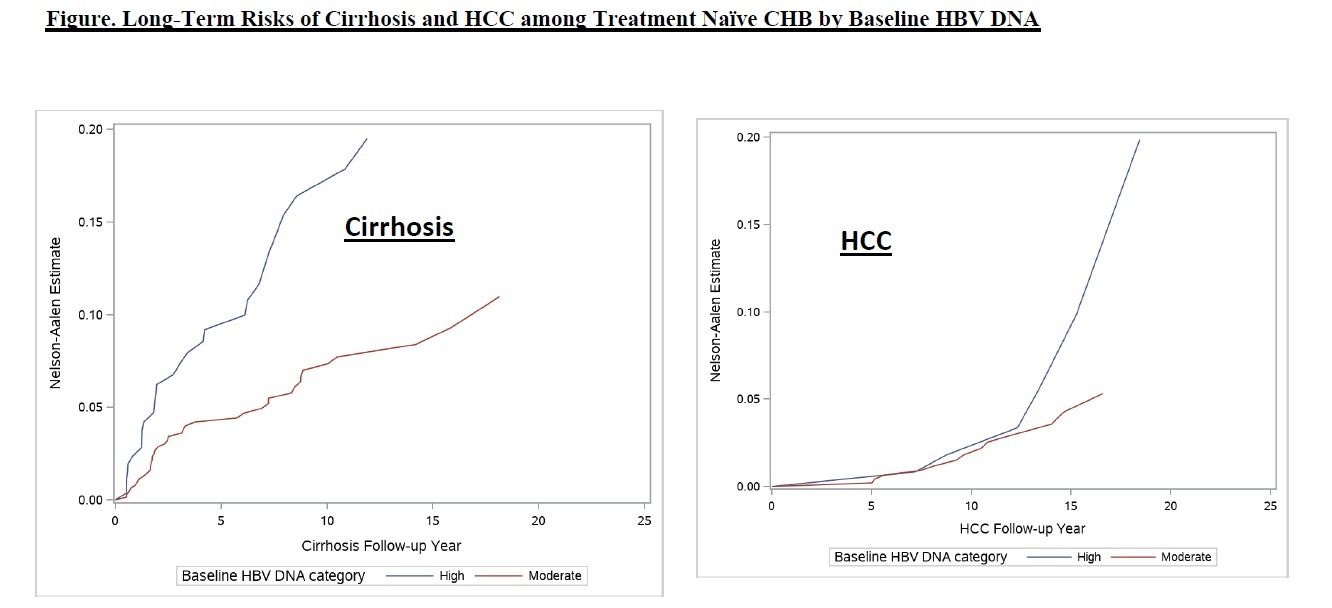
Figure: Figure 1
Disclosures:
Zeyuan Yang indicated no relevant financial relationships.
Ramsey Cheung indicated no relevant financial relationships.
Janice Jou: Gilead Sciences – Grant/Research Support.
Joseph Lim: Gilead Sciences – Grant/Research Support. Intercept – Grant/Research Support. Inventiva – Grant/Research Support. Novo Nordisk – Grant/Research Support. Pfizer – Grant/Research Support. Viking Therapeutics – Grant/Research Support.
Robert Wong: Durect Corporation – Grant/Research Support. Exact Sciences – Grant/Research Support. Gilead Sciences – Grant/Research Support. Thera Technologies – Grant/Research Support.
Zeyuan Yang, MS1, Ramsey Cheung, MD2, Janice Jou, MD3, Joseph Lim, MD4, Robert Wong, MD, MS, FACG5. P4592 - Long-Term Risks of Cirrhosis and Hepatocellular Carcinoma Among Treatment Naïve Chronic Hepatitis B Patients by Baseline Hepatitis B Viral Load, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
