Tuesday Poster Session
Category: Liver
P4605 - Non-English Primary Language Linked to Increased Complications and Reduced Transplant Rates in Cirrhosis Patients: Insights From Population-Based Multi-Network Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Khaled Alsabbagh Alchirazi, MD
Aurora Healthcare
Brookfield, WI
Presenting Author(s)
Award: ACG Health Equity Research Award
Award: Presidential Poster Award
Khaled Alsabbagh Alchirazi, MD1, Ahmed El Telbany, MD, MPH2, Mohamad-Noor Abu-Hammour, MD3, Nour Azzouz, MD4, Motasem Alkhayyat, MD4, Naim Alkhouri, MD5
1Aurora Healthcare, Brookfield, WI; 2University of New Mexico, Albuquerque, NM; 3Cleveland Clinic Fairview, Cleveland, OH; 4Cleveland Clinic, Cleveland, OH; 5Arizona Liver Health, Phoenix, AZ
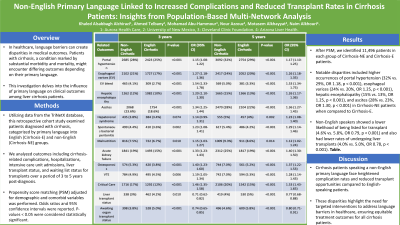
Introduction: In healthcare, language barriers can create disparities in medical outcomes. Patients with cirrhosis, a condition marked by substantial morbidity and mortality, might encounter differing outcomes depending on their primary language. This investigation delves into the influence of primary language on clinical outcomes among liver cirrhosis patients, specifically comparing non-English speaking (Cirrhosis-NE) individuals with their English-speaking counterparts (Cirrhosis-E).
Methods: Utilizing data from the TriNetX federated health research database, this retrospective cohort study examined patients diagnosed with cirrhosis, categorized by primary language into English (Cirrhosis-E) and non-English (Cirrhosis-NE) groups. We analyzed outcomes including cirrhosis-related complications, hospitalizations, intensive care unit admissions, liver transplant status, and waiting list status for transplants over a period of 3 to 5 years post-diagnosis. Propensity score matching adjusted for demographic and comorbid variables, ensuring comparability between groups. Statistical significance was determined using t-tests, chi-square/Fisher's exact tests. Odds ratios and 95% confidence intervals were reported. P-values < 0.05 were considered statistically significant.
Results: After propensity matching score, we identified 11,496 patients in each group of Cirrhosis-NE and Cirrhosis-E patients. Notable disparities included higher occurrences of portal hypertension (32% vs. 29%, OR 1.18, p < 0.001), esophageal varices (24% vs. 20%, OR 1.25, p < 0.001), hepatic encephalopathy (15% vs. 13%, OR 1.25, p < 0.001), and ascites (28% vs. 23%, OR 1.30, p < 0.001) in Cirrhosis-NE patients when compared to Cirrhosis-E. Moreover, non-English speakers showed a lower likelihood of being listed for transplant (4.6% vs. 5.8%, OR 0.79, p < 0.001) and also had lower rates of undergoing liver transplants (4.0% vs. 5.0%, OR 0.78, p < 0.001). Table1.
Discussion: Cirrhosis patients speaking a non-English primary language face heightened complication rates and reduced transplant opportunities compared to English-speaking patients. These disparities highlight the need for targeted interventions to address language barriers in healthcare, ensuring equitable treatment outcomes for all cirrhosis patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Alsabbagh Alchirazi, MD1, Ahmed El Telbany, MD, MPH2, Mohamad-Noor Abu-Hammour, MD3, Nour Azzouz, MD4, Motasem Alkhayyat, MD4, Naim Alkhouri, MD5. P4605 - Non-English Primary Language Linked to Increased Complications and Reduced Transplant Rates in Cirrhosis Patients: Insights From Population-Based Multi-Network Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Award: Presidential Poster Award
Khaled Alsabbagh Alchirazi, MD1, Ahmed El Telbany, MD, MPH2, Mohamad-Noor Abu-Hammour, MD3, Nour Azzouz, MD4, Motasem Alkhayyat, MD4, Naim Alkhouri, MD5
1Aurora Healthcare, Brookfield, WI; 2University of New Mexico, Albuquerque, NM; 3Cleveland Clinic Fairview, Cleveland, OH; 4Cleveland Clinic, Cleveland, OH; 5Arizona Liver Health, Phoenix, AZ
Introduction: In healthcare, language barriers can create disparities in medical outcomes. Patients with cirrhosis, a condition marked by substantial morbidity and mortality, might encounter differing outcomes depending on their primary language. This investigation delves into the influence of primary language on clinical outcomes among liver cirrhosis patients, specifically comparing non-English speaking (Cirrhosis-NE) individuals with their English-speaking counterparts (Cirrhosis-E).
Methods: Utilizing data from the TriNetX federated health research database, this retrospective cohort study examined patients diagnosed with cirrhosis, categorized by primary language into English (Cirrhosis-E) and non-English (Cirrhosis-NE) groups. We analyzed outcomes including cirrhosis-related complications, hospitalizations, intensive care unit admissions, liver transplant status, and waiting list status for transplants over a period of 3 to 5 years post-diagnosis. Propensity score matching adjusted for demographic and comorbid variables, ensuring comparability between groups. Statistical significance was determined using t-tests, chi-square/Fisher's exact tests. Odds ratios and 95% confidence intervals were reported. P-values < 0.05 were considered statistically significant.
Results: After propensity matching score, we identified 11,496 patients in each group of Cirrhosis-NE and Cirrhosis-E patients. Notable disparities included higher occurrences of portal hypertension (32% vs. 29%, OR 1.18, p < 0.001), esophageal varices (24% vs. 20%, OR 1.25, p < 0.001), hepatic encephalopathy (15% vs. 13%, OR 1.25, p < 0.001), and ascites (28% vs. 23%, OR 1.30, p < 0.001) in Cirrhosis-NE patients when compared to Cirrhosis-E. Moreover, non-English speakers showed a lower likelihood of being listed for transplant (4.6% vs. 5.8%, OR 0.79, p < 0.001) and also had lower rates of undergoing liver transplants (4.0% vs. 5.0%, OR 0.78, p < 0.001). Table1.
Discussion: Cirrhosis patients speaking a non-English primary language face heightened complication rates and reduced transplant opportunities compared to English-speaking patients. These disparities highlight the need for targeted interventions to address language barriers in healthcare, ensuring equitable treatment outcomes for all cirrhosis patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Khaled Alsabbagh Alchirazi indicated no relevant financial relationships.
Ahmed El Telbany indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Nour Azzouz indicated no relevant financial relationships.
Motasem Alkhayyat indicated no relevant financial relationships.
Naim Alkhouri: 89Bio – Grant/Research Support. Akero – Advisory Committee/Board Member, Grant/Research Support. Boehringer Ingelheim – Advisory Committee/Board Member, Grant/Research Support. Gilead – Grant/Research Support, Speakers Bureau. Inventiva – Grant/Research Support. Ipsen – Consultant, Grant/Research Support, Speakers Bureau. Madrigal – Advisory Committee/Board Member, Grant/Research Support, Speakers Bureau. Novo Nordisk – Grant/Research Support.
Khaled Alsabbagh Alchirazi, MD1, Ahmed El Telbany, MD, MPH2, Mohamad-Noor Abu-Hammour, MD3, Nour Azzouz, MD4, Motasem Alkhayyat, MD4, Naim Alkhouri, MD5. P4605 - Non-English Primary Language Linked to Increased Complications and Reduced Transplant Rates in Cirrhosis Patients: Insights From Population-Based Multi-Network Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

