Tuesday Poster Session
Category: Liver
P4607 - Disparities in Locoregional Therapy Type or Curative Intent for Hepatocellular Carcinoma by Race or Ethnicity
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sydney Power, MD
University of North Carolina
Chapel Hill, NC
Presenting Author(s)
Sydney Power, MD1, Yue Jiang, PhD2, Chidi Iloabachie, BS3, Arjun Juneja, BS4, Merete Lund, MD1, Gabe Lupu, MD1, Joyce Badal, MD4, David Seligson, MS5, Hanna Sanoff, MD1, David Mauro, MD1, David Gerber, MD6, Ted Yanagihara, MD1, A. Sidney Barritt, MD, MSCR1, Andrew Moon, MD, MPH1
1University of North Carolina, Chapel Hill, NC; 2Duke University, Chapel Hill, NC; 3University of North Carolina at Chapel Hill School of Medicine, Carrboro, NC; 4University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 5Center for Gastrointestinal Biology and Disease, University of North Carolina, Chapel Hill, NC; 6University of Cincinnati, Chapel Hill, NC
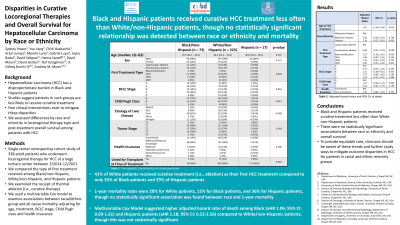
Introduction: Hepatocellular carcinoma (HCC) has a disproportionate burden in Black and Hispanic patients. Studies have suggested that patients in such groups are less likely to receive curative treatment, and few clinical implications exist to mitigate these disparities. To better understand potential inequities in HCC treatment, we aimed to characterize disparities along racial and ethnic lines in locoregional therapy type or curative intent for HCC in a single tertiary care center.
Methods: We conducted a single center retrospective cohort study of 338 adult patients who underwent locoregional therapy for HCC at a large tertiary center between 1/1/2014 and 12/31/2021. Treatment types include laparoscopic ablation, percutaneous ablation, bland embolization, transarterial chemoembolization (TACE), transarterial radioembolization (TARE/Y90), and stereotactic body radiation therapy (SBRT). We compared the type of first treatment received among Black/non-Hispanic, White/non-Hispanic, and Hispanic patients. We used a multivariable Cox model to examine associations between racial/ethnic group and death, adjusting for age, treatment, BCLC stage, Child Pugh class and type of medical insurance.
Results: Of the 338 patients, 73 were identified as Black/non-Hispanic, 223 were identified as White/non-Hispanic, 17 were identified as Hispanic, and 25 did not identify in any these categories. The multivariable Cox model for suggested higher hazard of death among patients undergoing bland embolization vs. laparoscopic ablation (adjusted hazard ratio (aHR) 2.51; 95% CI: 1.06 – 5.95) and patients in BCLC stage B vs. stage 0 (aHR 2.21; 95% CI: 1.08 – 4.52). Although adjusted hazard of death was higher among Black/non-Hispanic (aHR 1.06; 95% CI: 0.69 – 1.61) and Hispanic (aHR 1.18; 95% CI: 0.52 – 2.65) patients compared to White non-Hispanic patients, this was not a statistically significant difference.
Discussion: Although Black and Hispanic patients received curative treatment less often than White non-Hispanic patients, we failed to detect a statistically significant relationship between race/ethnicity and death. Regardless, to provide equitable care, clinicians should be aware of these trends and further study ways to mitigate outcome disparities in HCC for patients in racial and ethnic minority groups.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sydney Power, MD1, Yue Jiang, PhD2, Chidi Iloabachie, BS3, Arjun Juneja, BS4, Merete Lund, MD1, Gabe Lupu, MD1, Joyce Badal, MD4, David Seligson, MS5, Hanna Sanoff, MD1, David Mauro, MD1, David Gerber, MD6, Ted Yanagihara, MD1, A. Sidney Barritt, MD, MSCR1, Andrew Moon, MD, MPH1. P4607 - Disparities in Locoregional Therapy Type or Curative Intent for Hepatocellular Carcinoma by Race or Ethnicity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Carolina, Chapel Hill, NC; 2Duke University, Chapel Hill, NC; 3University of North Carolina at Chapel Hill School of Medicine, Carrboro, NC; 4University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 5Center for Gastrointestinal Biology and Disease, University of North Carolina, Chapel Hill, NC; 6University of Cincinnati, Chapel Hill, NC
Introduction: Hepatocellular carcinoma (HCC) has a disproportionate burden in Black and Hispanic patients. Studies have suggested that patients in such groups are less likely to receive curative treatment, and few clinical implications exist to mitigate these disparities. To better understand potential inequities in HCC treatment, we aimed to characterize disparities along racial and ethnic lines in locoregional therapy type or curative intent for HCC in a single tertiary care center.
Methods: We conducted a single center retrospective cohort study of 338 adult patients who underwent locoregional therapy for HCC at a large tertiary center between 1/1/2014 and 12/31/2021. Treatment types include laparoscopic ablation, percutaneous ablation, bland embolization, transarterial chemoembolization (TACE), transarterial radioembolization (TARE/Y90), and stereotactic body radiation therapy (SBRT). We compared the type of first treatment received among Black/non-Hispanic, White/non-Hispanic, and Hispanic patients. We used a multivariable Cox model to examine associations between racial/ethnic group and death, adjusting for age, treatment, BCLC stage, Child Pugh class and type of medical insurance.
Results: Of the 338 patients, 73 were identified as Black/non-Hispanic, 223 were identified as White/non-Hispanic, 17 were identified as Hispanic, and 25 did not identify in any these categories. The multivariable Cox model for suggested higher hazard of death among patients undergoing bland embolization vs. laparoscopic ablation (adjusted hazard ratio (aHR) 2.51; 95% CI: 1.06 – 5.95) and patients in BCLC stage B vs. stage 0 (aHR 2.21; 95% CI: 1.08 – 4.52). Although adjusted hazard of death was higher among Black/non-Hispanic (aHR 1.06; 95% CI: 0.69 – 1.61) and Hispanic (aHR 1.18; 95% CI: 0.52 – 2.65) patients compared to White non-Hispanic patients, this was not a statistically significant difference.
Discussion: Although Black and Hispanic patients received curative treatment less often than White non-Hispanic patients, we failed to detect a statistically significant relationship between race/ethnicity and death. Regardless, to provide equitable care, clinicians should be aware of these trends and further study ways to mitigate outcome disparities in HCC for patients in racial and ethnic minority groups.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sydney Power indicated no relevant financial relationships.
Yue Jiang indicated no relevant financial relationships.
Chidi Iloabachie indicated no relevant financial relationships.
Arjun Juneja indicated no relevant financial relationships.
Merete Lund indicated no relevant financial relationships.
Gabe Lupu indicated no relevant financial relationships.
Joyce Badal indicated no relevant financial relationships.
David Seligson indicated no relevant financial relationships.
Hanna Sanoff: Amgen – Grant/Research Support. AstraZeneca – Grant/Research Support. Biomed Valley Discoveries – Grant/Research Support. Bristol-Myers Squibb – Grant/Research Support. Exelis – Grant/Research Support. F Hoffman La Roche – Grant/Research Support. Pfizer – Grant/Research Support. Rgenix – Grant/Research Support.
David Mauro indicated no relevant financial relationships.
David Gerber: Medtronic – Consultant.
Ted Yanagihara indicated no relevant financial relationships.
A. Sidney Barritt: TARGET RWE – Consultant.
Andrew Moon: DCN Diagnostics – Grant/Research Support. Intercept – Advisory Committee/Board Member. TARGET RWE – Consultant.
Sydney Power, MD1, Yue Jiang, PhD2, Chidi Iloabachie, BS3, Arjun Juneja, BS4, Merete Lund, MD1, Gabe Lupu, MD1, Joyce Badal, MD4, David Seligson, MS5, Hanna Sanoff, MD1, David Mauro, MD1, David Gerber, MD6, Ted Yanagihara, MD1, A. Sidney Barritt, MD, MSCR1, Andrew Moon, MD, MPH1. P4607 - Disparities in Locoregional Therapy Type or Curative Intent for Hepatocellular Carcinoma by Race or Ethnicity, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
