Tuesday Poster Session
Category: Liver
P4661 - Treatment Perceptions and Experiences Among Patients With PBC: Qualitative Results From the ITCH-E Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CM
C. Fiorella Murillo Perez, PhD
Gilead Sciences, Inc.
Foster City, CA
Presenting Author(s)
Cynthia Levy, MD1, Zobair Younossi, MD, MPH, FACG2, Jonathan Ieyoub, MS, NP3, Rebekah Zincavage, PhD4, Brad Padilla, MPH4, Diane Ito, MA4, C. Fiorella Murillo Perez, PhD3
1University of Miami, Miami, FL; 2The Global NASH Council, Washington, DC; 3Gilead Sciences, Inc., Foster City, CA; 4Stratevi, Santa Monica, CA
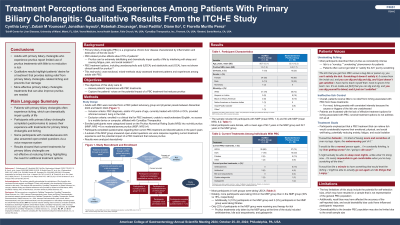
Introduction: Individuals living with primary biliary cholangitis (PBC) often experience debilitating symptoms such as pruritus. Current PBC treatments may fail to alleviate pruritus, which can hinder providing optimal care. This study assessed treatment patterns and experiences among adults with PBC.
Methods: Adults with PBC were recruited from a PBC patient advocacy group and physician panels between 12/23 and 03/24. Enrolled participants were categorized based on the Pruritus Numerical Rating Scale (NRS) into no/mild pruritus (NMP, NRS< 4) vs. moderate/severe pruritus (MSP, NRS?4). Participants completed questions regarding their current PBC treatment and discontinuations in the past 3 years. A subset of the MSP group answered open-ended questions regarding current treatment experience and the potential impact of a PBC treatment that reduces pruritus via voice response. Results were analyzed descriptively.
Results: The sample included 40 NMP (mean NRS 1.3) and 50 MSP (mean NRS 6.2) participants with a mean age of 56.7 and 52.1 with 85% and 80% female participants, respectively. NMP and MSP groups included 78% and 72% White, 8% and 16% Latino, 8% and 10% Black, 3% and 0% Native American, 0% and 6% Asian, 20% and 8% Other, respectively. Most in both groups were taking ursodeoxycholic acid (UDCA), 88% and 74%, respectively. Notably, more MSP participants were taking obeticholic acid (OCA) than those in the NMP group (30% vs 18%). Of those who discontinued OCA in past 3 years (n=6), reasons included ineffectiveness (50%), side effects (17%), doctor recommended discontinuing (17%) and other (17%). Only 22% of patients in the MSP group were receiving any therapy for itch. Pruritus treatments currently only taken by the MSP group included: antihistamines, bile acid sequestrants, and gabapentin (Table 1). Patient voice data stressed the poor effectiveness and short duration of current treatments for pruritus due to PBC, causing frustration. Most described their pruritus as consistently intense. They emphasized that a PBC treatment that can relieve itch would considerably improve their emotional, physical, and social well-being, potentially reducing anxiety, fatigue, and social isolation.
Discussion: Adults with PBC who suffer from pruritus report limited use of pruritus treatments with little to no reduction in itch. There is a clear unmet need for more effective PBC treatments that can also improve pruritus.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Cynthia Levy, MD1, Zobair Younossi, MD, MPH, FACG2, Jonathan Ieyoub, MS, NP3, Rebekah Zincavage, PhD4, Brad Padilla, MPH4, Diane Ito, MA4, C. Fiorella Murillo Perez, PhD3. P4661 - Treatment Perceptions and Experiences Among Patients With PBC: Qualitative Results From the ITCH-E Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Miami, Miami, FL; 2The Global NASH Council, Washington, DC; 3Gilead Sciences, Inc., Foster City, CA; 4Stratevi, Santa Monica, CA
Introduction: Individuals living with primary biliary cholangitis (PBC) often experience debilitating symptoms such as pruritus. Current PBC treatments may fail to alleviate pruritus, which can hinder providing optimal care. This study assessed treatment patterns and experiences among adults with PBC.
Methods: Adults with PBC were recruited from a PBC patient advocacy group and physician panels between 12/23 and 03/24. Enrolled participants were categorized based on the Pruritus Numerical Rating Scale (NRS) into no/mild pruritus (NMP, NRS< 4) vs. moderate/severe pruritus (MSP, NRS?4). Participants completed questions regarding their current PBC treatment and discontinuations in the past 3 years. A subset of the MSP group answered open-ended questions regarding current treatment experience and the potential impact of a PBC treatment that reduces pruritus via voice response. Results were analyzed descriptively.
Results: The sample included 40 NMP (mean NRS 1.3) and 50 MSP (mean NRS 6.2) participants with a mean age of 56.7 and 52.1 with 85% and 80% female participants, respectively. NMP and MSP groups included 78% and 72% White, 8% and 16% Latino, 8% and 10% Black, 3% and 0% Native American, 0% and 6% Asian, 20% and 8% Other, respectively. Most in both groups were taking ursodeoxycholic acid (UDCA), 88% and 74%, respectively. Notably, more MSP participants were taking obeticholic acid (OCA) than those in the NMP group (30% vs 18%). Of those who discontinued OCA in past 3 years (n=6), reasons included ineffectiveness (50%), side effects (17%), doctor recommended discontinuing (17%) and other (17%). Only 22% of patients in the MSP group were receiving any therapy for itch. Pruritus treatments currently only taken by the MSP group included: antihistamines, bile acid sequestrants, and gabapentin (Table 1). Patient voice data stressed the poor effectiveness and short duration of current treatments for pruritus due to PBC, causing frustration. Most described their pruritus as consistently intense. They emphasized that a PBC treatment that can relieve itch would considerably improve their emotional, physical, and social well-being, potentially reducing anxiety, fatigue, and social isolation.
Discussion: Adults with PBC who suffer from pruritus report limited use of pruritus treatments with little to no reduction in itch. There is a clear unmet need for more effective PBC treatments that can also improve pruritus.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Cynthia Levy: Calliditas – Consultant. CymaBay, a Gilead Sciences Company – Consultant. GSK – Consultant. Intercept – Consultant. Ipsen – Consultant. Kowa Pharmaceuticals – Consultant. Mirum – Consultant.
Zobair Younossi: Intercept, Cymabay, Boehringer Ingelheim, Ipsen, BMS, GSK, NovoNordisk, Merck and Abbott. – Grant/Research Support. Madrigal – Grant/Research Support. Siemens – Grant/Research Support.
Jonathan Ieyoub: Gilead Sciences – Employee.
Rebekah Zincavage: Gilead Sciences – Consultant.
Brad Padilla: Gilead Sciences – Consultant.
Diane Ito: Gilead Sciences – Consultant.
C. Fiorella Murillo Perez: Gilead Sciences – Employee.
Cynthia Levy, MD1, Zobair Younossi, MD, MPH, FACG2, Jonathan Ieyoub, MS, NP3, Rebekah Zincavage, PhD4, Brad Padilla, MPH4, Diane Ito, MA4, C. Fiorella Murillo Perez, PhD3. P4661 - Treatment Perceptions and Experiences Among Patients With PBC: Qualitative Results From the ITCH-E Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
