Tuesday Poster Session
Category: Liver
P4696 - Epstein-Barr Virus and Herpes Simplex Virus Co-Infection: A Rare Cause of Severe Acute Liver Injury
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- VK
Vyshnavi Kodali, DO
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Vyshnavi Kodali, DO1, Konstantinos Damiris, DO1, Bing Chen, MD2, Alberto Unzueta, MD3
1Geisinger Medical Center, Danville, PA; 2Geisenger Medical Center, Danville, PA; 3Geisinger Medical Center, Lewisburg, PA
Introduction: Epstein-Barr Virus (EBV) & Herpes Simplex Virus (HSV) co-infection is a rare cause of acute liver injury, with limited reported cases in the current literature. As viral hepatitis induced acute liver injury can progress to acute liver failure (ALF), early hepatology consult is warranted.
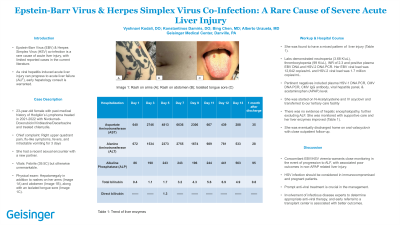
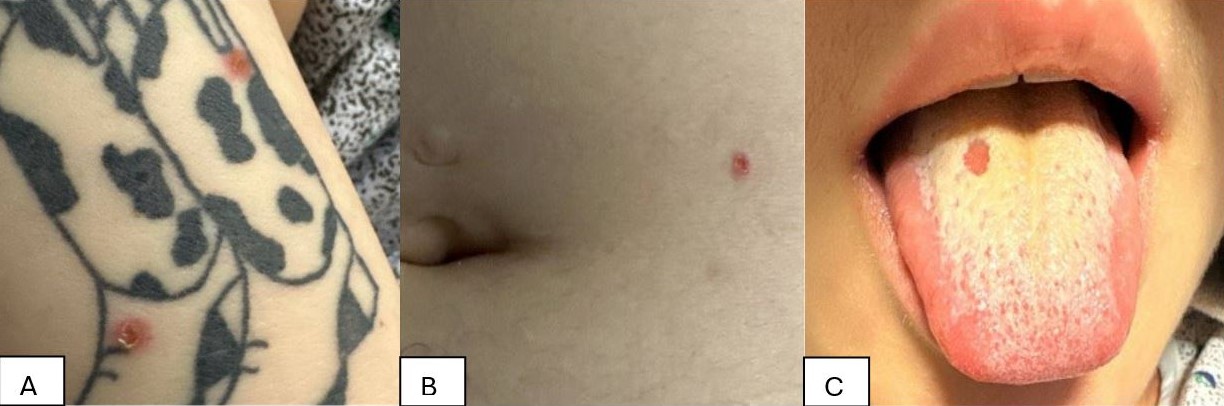
Case Description/Methods: This patient is a 23-year-old female with past medical history of Hodgkin’s Lymphoma treated in 2021-2022 with Nivolumab-Doxorubicin/Vinblastine/Dacarbazine and treated chlamydia. She initially presented with chief complaint of right upper quadrant pain, flu-like symptoms, fevers, and intractable vomiting for 3 days with minimal relief with over-the-counter naproxen. History was significant for a recent sexual encounter with a new partner. She was febrile (39.5 C) but vital signs were otherwise unremarkable. Physical exam revealed hepatomegaly in addition to rashes on her arms (Image 1A) and abdomen (Image 1B), along with an isolated tongue sore (Image 1C). She was found to have hepatocellular and cholestatic pattern of liver injury (Table 1). Labs showed neutropenia (3.68 K/uL), thrombocytopenia (99 K/uL), INR of 2.3 and positive plasma EBV DNA and HSV-2 DNA PCR. Her EBV viral load was 12,642 copies/mL and HSV-2 viral load was 1.7 million copies/mL. Pertinent negatives included plasma HSV-1 DNA PCR, CMV DNA PCR, CMV IgG antibody, viral hepatitis panel, & acetaminophen (APAP) level. She was started on N-Acetylcysteine and transferred to our tertiary care center for further evaluation. She was started on IV acyclovir. Her hospital course was complicated by multiple episodes of hypoglycemia, likely secondary to impaired gluconeogenesis in the setting of acute liver injury. There was no evidence of hepatic encephalopathy, further excluding ALF. She was monitored with supportive care and her liver enzymes improved (Table 1). She was eventually discharged home on oral valacyclovir with close outpatient follow-up.
Discussion: Concomitant EBV/HSV viremia is an uncommon cause of severe acute liver injury and warrants close monitoring in the event of progression to ALF, with associated poor outcomes in non-APAP related liver injury. HSV infection should especially be considered in immunocompromised and pregnant patients and prompt anti-viral treatment is crucial in the management. Involvement of infectious disease experts to determine appropriate anti-viral therapy, and early referral to a transplant center is associated with better outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Vyshnavi Kodali, DO1, Konstantinos Damiris, DO1, Bing Chen, MD2, Alberto Unzueta, MD3. P4696 - Epstein-Barr Virus and Herpes Simplex Virus Co-Infection: A Rare Cause of Severe Acute Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Geisinger Medical Center, Danville, PA; 2Geisenger Medical Center, Danville, PA; 3Geisinger Medical Center, Lewisburg, PA
Introduction: Epstein-Barr Virus (EBV) & Herpes Simplex Virus (HSV) co-infection is a rare cause of acute liver injury, with limited reported cases in the current literature. As viral hepatitis induced acute liver injury can progress to acute liver failure (ALF), early hepatology consult is warranted.
Case Description/Methods: This patient is a 23-year-old female with past medical history of Hodgkin’s Lymphoma treated in 2021-2022 with Nivolumab-Doxorubicin/Vinblastine/Dacarbazine and treated chlamydia. She initially presented with chief complaint of right upper quadrant pain, flu-like symptoms, fevers, and intractable vomiting for 3 days with minimal relief with over-the-counter naproxen. History was significant for a recent sexual encounter with a new partner. She was febrile (39.5 C) but vital signs were otherwise unremarkable. Physical exam revealed hepatomegaly in addition to rashes on her arms (Image 1A) and abdomen (Image 1B), along with an isolated tongue sore (Image 1C). She was found to have hepatocellular and cholestatic pattern of liver injury (Table 1). Labs showed neutropenia (3.68 K/uL), thrombocytopenia (99 K/uL), INR of 2.3 and positive plasma EBV DNA and HSV-2 DNA PCR. Her EBV viral load was 12,642 copies/mL and HSV-2 viral load was 1.7 million copies/mL. Pertinent negatives included plasma HSV-1 DNA PCR, CMV DNA PCR, CMV IgG antibody, viral hepatitis panel, & acetaminophen (APAP) level. She was started on N-Acetylcysteine and transferred to our tertiary care center for further evaluation. She was started on IV acyclovir. Her hospital course was complicated by multiple episodes of hypoglycemia, likely secondary to impaired gluconeogenesis in the setting of acute liver injury. There was no evidence of hepatic encephalopathy, further excluding ALF. She was monitored with supportive care and her liver enzymes improved (Table 1). She was eventually discharged home on oral valacyclovir with close outpatient follow-up.
Discussion: Concomitant EBV/HSV viremia is an uncommon cause of severe acute liver injury and warrants close monitoring in the event of progression to ALF, with associated poor outcomes in non-APAP related liver injury. HSV infection should especially be considered in immunocompromised and pregnant patients and prompt anti-viral treatment is crucial in the management. Involvement of infectious disease experts to determine appropriate anti-viral therapy, and early referral to a transplant center is associated with better outcomes.
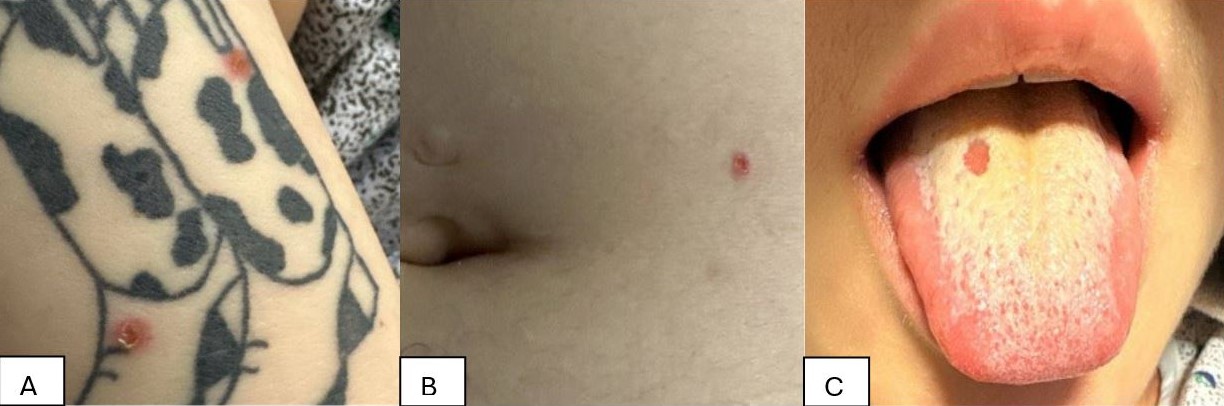
Figure: Image 1: Physical Exam Findings
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Vyshnavi Kodali indicated no relevant financial relationships.
Konstantinos Damiris indicated no relevant financial relationships.
Bing Chen indicated no relevant financial relationships.
Alberto Unzueta indicated no relevant financial relationships.
Vyshnavi Kodali, DO1, Konstantinos Damiris, DO1, Bing Chen, MD2, Alberto Unzueta, MD3. P4696 - Epstein-Barr Virus and Herpes Simplex Virus Co-Infection: A Rare Cause of Severe Acute Liver Injury, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

