Tuesday Poster Session
Category: Liver
P4706 - Yersinia Enterocolitica Hepatic Abscesses Masquerading as Hepatic Metastases
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Jonathan Rozenberg, DO, MPH
Carilion Clinic
Roanoke, VA
Presenting Author(s)
Jonathan Rozenberg, DO, MPH1, Adil Mir, MD1, Joel Joseph, MD1, Diana Dougherty, MD1, Klaus Monkemuller, MD, PhD2, Vivek Kesar, MD1
1Carilion Clinic, Roanoke, VA; 2Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: Yersinia enterocolitica (YE) is a gram-negative bacillus found in water, soil, or intestinal tracts of animals with a fecal-oral mechanism of transmission to humans. Typical presentation of YE infection includes bloody vs mucoid diarrhea, abdominal pain, or fever. Severe disease (e.g., septicemia, hepatic/splenic abscesses) has been reported in the literature in those with risk factors: hepatic disease, diabetes mellitus, iron overload state (e.g., hemochromatosis), or immunosuppression. Cases of YE hepatic abscesses are uncommon within the literature and are often a sequalae of enteric disease (e.g., enterocolitis, mesenteric adenitis, or terminal ileitis). We present a rare case of YE hepatic abscesses initially thought to be hepatic metastases.
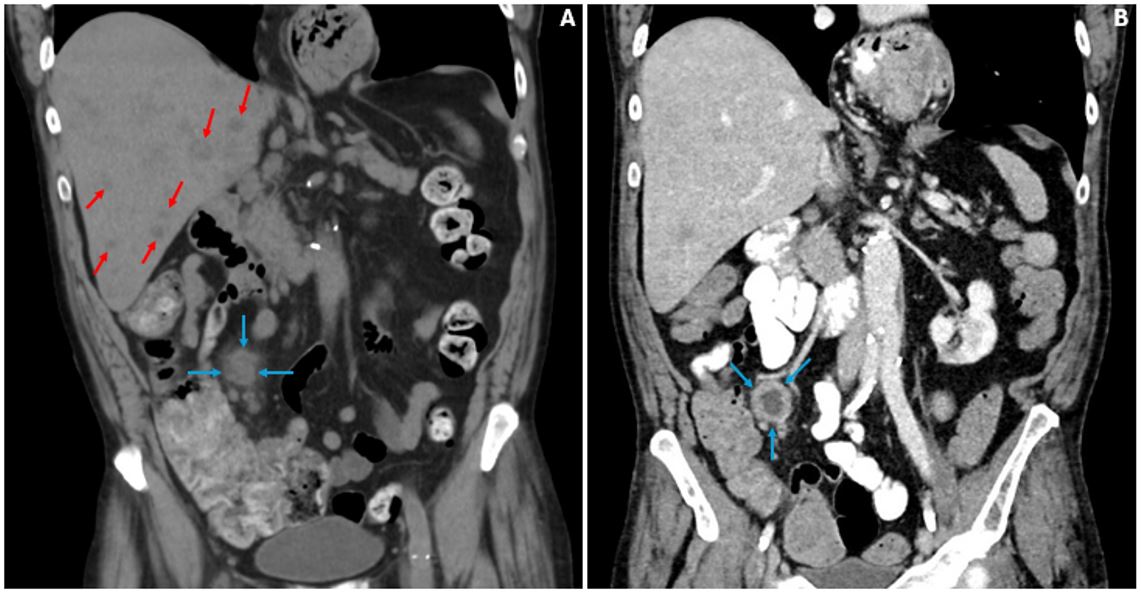
Case Description/Methods: A 64-year-old male presented with generalized abdominal pain. Past medical history was significant for laryngeal carcinoma status post total laryngectomy and XRT (2009). Physical exam was unrevealing. Pertinent labs were as follows: Ferritin 672.7 ng/mL (reference 30-400 ng/mL), TSAT 10% (reference 9.2-49.1%), Hemoglobin A1c 8.5%. CT Abdomen/Pelvis found a new 2.8 cm nonspecific thick-walled hypodense lesion in the RLQ with peripheral enhancement, adjacent prominent lymph nodes and innumerable hypoattenuating lesions within the liver (Figure 1) concerning for metastatic disease, which was supported by PET/CT. Liver biopsy was consistent with abscess on pathology. Biopsy culture grew Yersinia enterocolitica with resistance to ampicillin, cefazolin. He was started on cefepime, metronidazole and then discharged on levofloxacin, metronidazole for a combined total of 3 weeks. All other culture studies including urine, blood, and stool were negative. No large lesion or mass was seen on colonoscopy. Outpatient repeat imaging saw interval resolution of the hepatic lesions (Figure 1) and the RLQ lesion was found to be an abscess upon biopsy.
Discussion: Multiple hepatic lesions provide a differential mainly consisting of abscesses vs metastases vs cysts. The most common comorbidities reported among cases of YE hepatic abscesses are hemochromatosis (~60%) and diabetes mellitus (~30%). Our patient was noted to have elevated HbA1c of 8.5% as a risk factor. This case highlights this rare clinical entity and serves as a reminder to consider rare differentials in such cases.
Disclosures:
Jonathan Rozenberg, DO, MPH1, Adil Mir, MD1, Joel Joseph, MD1, Diana Dougherty, MD1, Klaus Monkemuller, MD, PhD2, Vivek Kesar, MD1. P4706 - Yersinia Enterocolitica Hepatic Abscesses Masquerading as Hepatic Metastases, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Carilion Clinic, Roanoke, VA; 2Virginia Tech Carilion School of Medicine, Roanoke, VA
Introduction: Yersinia enterocolitica (YE) is a gram-negative bacillus found in water, soil, or intestinal tracts of animals with a fecal-oral mechanism of transmission to humans. Typical presentation of YE infection includes bloody vs mucoid diarrhea, abdominal pain, or fever. Severe disease (e.g., septicemia, hepatic/splenic abscesses) has been reported in the literature in those with risk factors: hepatic disease, diabetes mellitus, iron overload state (e.g., hemochromatosis), or immunosuppression. Cases of YE hepatic abscesses are uncommon within the literature and are often a sequalae of enteric disease (e.g., enterocolitis, mesenteric adenitis, or terminal ileitis). We present a rare case of YE hepatic abscesses initially thought to be hepatic metastases.
Case Description/Methods: A 64-year-old male presented with generalized abdominal pain. Past medical history was significant for laryngeal carcinoma status post total laryngectomy and XRT (2009). Physical exam was unrevealing. Pertinent labs were as follows: Ferritin 672.7 ng/mL (reference 30-400 ng/mL), TSAT 10% (reference 9.2-49.1%), Hemoglobin A1c 8.5%. CT Abdomen/Pelvis found a new 2.8 cm nonspecific thick-walled hypodense lesion in the RLQ with peripheral enhancement, adjacent prominent lymph nodes and innumerable hypoattenuating lesions within the liver (Figure 1) concerning for metastatic disease, which was supported by PET/CT. Liver biopsy was consistent with abscess on pathology. Biopsy culture grew Yersinia enterocolitica with resistance to ampicillin, cefazolin. He was started on cefepime, metronidazole and then discharged on levofloxacin, metronidazole for a combined total of 3 weeks. All other culture studies including urine, blood, and stool were negative. No large lesion or mass was seen on colonoscopy. Outpatient repeat imaging saw interval resolution of the hepatic lesions (Figure 1) and the RLQ lesion was found to be an abscess upon biopsy.
Discussion: Multiple hepatic lesions provide a differential mainly consisting of abscesses vs metastases vs cysts. The most common comorbidities reported among cases of YE hepatic abscesses are hemochromatosis (~60%) and diabetes mellitus (~30%). Our patient was noted to have elevated HbA1c of 8.5% as a risk factor. This case highlights this rare clinical entity and serves as a reminder to consider rare differentials in such cases.
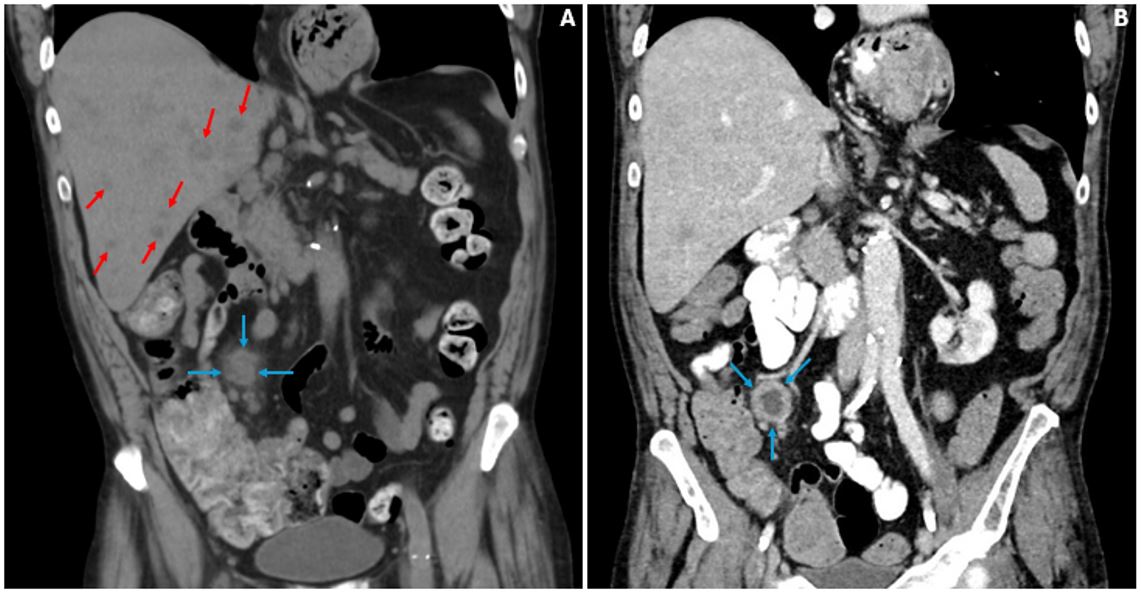
Figure: Figure 1: Panel A) CT showing RLQ lesion (blue arrows), hepatic lesions (red arrows), B) repeat CT with resolution of hepatic lesions, persistence of RLQ lesion (blue arrows)
Disclosures:
Jonathan Rozenberg indicated no relevant financial relationships.
Adil Mir indicated no relevant financial relationships.
Joel Joseph indicated no relevant financial relationships.
Diana Dougherty indicated no relevant financial relationships.
Klaus Monkemuller indicated no relevant financial relationships.
Vivek Kesar indicated no relevant financial relationships.
Jonathan Rozenberg, DO, MPH1, Adil Mir, MD1, Joel Joseph, MD1, Diana Dougherty, MD1, Klaus Monkemuller, MD, PhD2, Vivek Kesar, MD1. P4706 - Yersinia Enterocolitica Hepatic Abscesses Masquerading as Hepatic Metastases, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
