Tuesday Poster Session
Category: Liver
P4707 - A Case of Infected Loculated Ascites Managed with tPA Administration
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- NH
Nimra Hameed, MD
Stony Brook Medicine
Stony Brook, NY
Presenting Author(s)
Nimra Hameed, MD1, Daniel Carris, DO1, Isabella Pizzuto, BS2, Imran Baig, MD3
1Stony Brook Medicine, Stony Brook, NY; 2Renaissance School of Medicine at Stony Brook University, Stony Brook, NY; 3Northport VAMC, Northport, NY
Introduction: Spontaneous bacterial peritonitis (SBP) is an acute infection of ascites fluid related to liver cirrhosis which can be complicated by the development of infected loculations. We present a case of loculated infected ascites managed with alteplase (tPA).
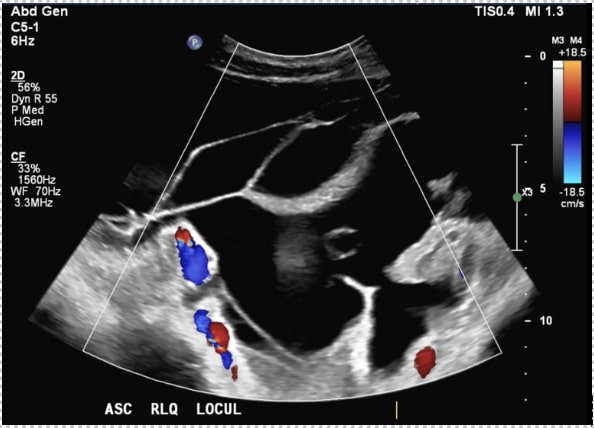
Case Description/Methods: Patient is a 59-year-old female with decompensated liver cirrhosis and pancreatic adenocarcinoma who presented with epigastric tenderness and spontaneous bacterial peritonitis (5301 WBCs and 86% neutrophils) despite rifaximin prophylaxis. Fluid grew Klebsiella pneumoniae treated with piperacillin-tazobactam. Day 3, patient was switched to cefepime due to mounting leukocytosis. Day 6, repeat diagnostic paracentesis had increased PMN count and antibiotics were switched to meropenem and vancomycin. Day 8, abdominal ultrasound revealed severe large volume complex loculated ascites throughout the abdomen (Figure 1). Given the nonresolution of patient’s SBP likely due to loculations, we decided to utilize tPA to lyse the septations. After initial placement of peritoneal drain, 3 liters were drained over 12 hours. After this 4mg of tPA was placed into patient’s abdomen and drain was clamped for 2 hours. The drain was opened resulting in 1L of fluid draining over 2 hours. Following administration of tPA, patient’s coagulation studies were stable. We had initially planned to repeat the instillation of tPA for 2 more days; however, further treatments were delayed by increasing fevers and leukocytosis.The patient later made plans for inpatient hospice given pancreatic adenocarcinoma.
Discussion:
When treating persistent SBP, infected loculations are a barrier to treatment and diagnostic and therapeutic paracenteses. The mechanism of loculations' development is unknown, it is proposed they develop through the deposition of fibrinogen and hypo-fibrinolysis due to liver cirrhosis. No current standardized protocol exists for the use of tPA for the management of loculated ascites. Treatment of loculated SBP presents a unique source control challenge, as drainage of individual pockets may be impractical. Utilizing tPA to break down loculations can introduce previously contained infection material into the peritoneal space can causing systemic inflammation and hemodynamic instability, as observed in this patient. This may limit further treatments with tPA.This case highlights the effectiveness of tPA in enhancing drainage of ascites fluid; however, it is unclear if it impacted efficacy of antibiotics for the treatment of SBP.
Disclosures:
Nimra Hameed, MD1, Daniel Carris, DO1, Isabella Pizzuto, BS2, Imran Baig, MD3. P4707 - A Case of Infected Loculated Ascites Managed with tPA Administration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Stony Brook Medicine, Stony Brook, NY; 2Renaissance School of Medicine at Stony Brook University, Stony Brook, NY; 3Northport VAMC, Northport, NY
Introduction: Spontaneous bacterial peritonitis (SBP) is an acute infection of ascites fluid related to liver cirrhosis which can be complicated by the development of infected loculations. We present a case of loculated infected ascites managed with alteplase (tPA).
Case Description/Methods: Patient is a 59-year-old female with decompensated liver cirrhosis and pancreatic adenocarcinoma who presented with epigastric tenderness and spontaneous bacterial peritonitis (5301 WBCs and 86% neutrophils) despite rifaximin prophylaxis. Fluid grew Klebsiella pneumoniae treated with piperacillin-tazobactam. Day 3, patient was switched to cefepime due to mounting leukocytosis. Day 6, repeat diagnostic paracentesis had increased PMN count and antibiotics were switched to meropenem and vancomycin. Day 8, abdominal ultrasound revealed severe large volume complex loculated ascites throughout the abdomen (Figure 1). Given the nonresolution of patient’s SBP likely due to loculations, we decided to utilize tPA to lyse the septations. After initial placement of peritoneal drain, 3 liters were drained over 12 hours. After this 4mg of tPA was placed into patient’s abdomen and drain was clamped for 2 hours. The drain was opened resulting in 1L of fluid draining over 2 hours. Following administration of tPA, patient’s coagulation studies were stable. We had initially planned to repeat the instillation of tPA for 2 more days; however, further treatments were delayed by increasing fevers and leukocytosis.The patient later made plans for inpatient hospice given pancreatic adenocarcinoma.
Discussion:
When treating persistent SBP, infected loculations are a barrier to treatment and diagnostic and therapeutic paracenteses. The mechanism of loculations' development is unknown, it is proposed they develop through the deposition of fibrinogen and hypo-fibrinolysis due to liver cirrhosis. No current standardized protocol exists for the use of tPA for the management of loculated ascites. Treatment of loculated SBP presents a unique source control challenge, as drainage of individual pockets may be impractical. Utilizing tPA to break down loculations can introduce previously contained infection material into the peritoneal space can causing systemic inflammation and hemodynamic instability, as observed in this patient. This may limit further treatments with tPA.This case highlights the effectiveness of tPA in enhancing drainage of ascites fluid; however, it is unclear if it impacted efficacy of antibiotics for the treatment of SBP.
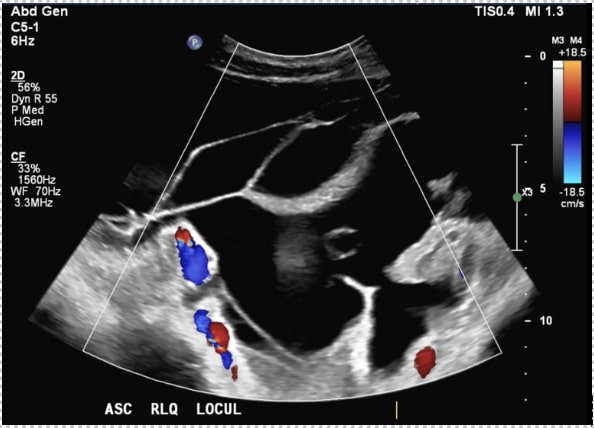
Figure: Figure 1
Disclosures:
Nimra Hameed indicated no relevant financial relationships.
Daniel Carris indicated no relevant financial relationships.
Isabella Pizzuto indicated no relevant financial relationships.
Imran Baig indicated no relevant financial relationships.
Nimra Hameed, MD1, Daniel Carris, DO1, Isabella Pizzuto, BS2, Imran Baig, MD3. P4707 - A Case of Infected Loculated Ascites Managed with tPA Administration, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

