Tuesday Poster Session
Category: Liver
P4721 - Complicated Portal Vein Thrombosis Requiring Creation of a Surgical Shunt
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- KL
Kim Minh Le, DO
Baylor Scott & White Medical Center
Austin, TX
Presenting Author(s)
Award: Presidential Poster Award
Kim Minh Le, DO1, Amar Gupta, MD2, Raja K. Dhanekula, MS, MD, MBBS3
1Baylor Scott & White Medical Center, Austin, TX; 2Baylor Scott & White Medical Center, Dallas, TX; 3Baylor Scott and White Round Rock, Round Rock, TX
Introduction: Portal vein thrombosis (PVT) is an uncommon condition with a prevalence of 0.7 to 1 per 100,000. Cavernous transformation of the portal vein (CTPV) is a complication of chronic PVT. The literature regarding CTPV is minimal, as most data is based on clinical series and case reports. We present a case of idiopathic PVT with CTPV complicated by non-cirrhotic portal hypertension (NCPH) manifested by recurrent esophageal variceal bleeding necessitating a surgical creation of a splenorenal shunt.
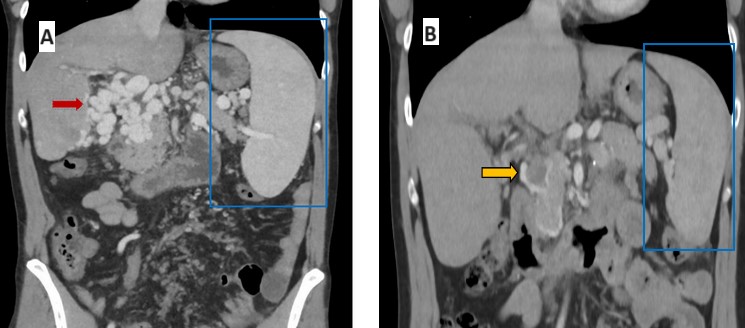
Case Description/Methods: The patient is a 37-year-old male who presented with easy bruising and was diagnosed with a PVT with CTPV. Despite preserved hepatic function, he had recurrent symptomatic anemia and melena for which he underwent four esophagogastroduodenoscopies, most revealing esophageal varices with high-risk stigmata requiring esophageal variceal ligations. He underwent a trial of non-selective beta blockers for secondary prophylaxis but unfortunately developed symptomatic hypotension. He was thus referred to transplant surgery for creation of a surgical shunt. Intraoperatively, the pressures in the splenic, superior mesenteric, and portal veins were 22 mmHg. A mesorectum shunt using the internal jugular vein was attempted to decompress the right sided portal hypertension but was unsuccessful. A splenorenal shunt was then created, decompressing both the left and right side of the spleno-mesenteric system. Pressures in the splenic vein and superior mesenteric vein dropped to 16 mmHg. The pressure in the left renal vein was 12 mmHg. This 4 mmHg porto-systemic gradient was expected to prevent bleeding from varices. Post-operative imaging showed a decrease in the upper abdominal varices and collateral vessels and near resolution of splenomegaly (15 cm to 12.5cm) and thrombocytopenia (58,000 to 132,000). There was evidence of a new thrombus within a collateral vessel near the pancreatic head, which supports functionality of the splenorenal shunt decreasing flow through the collaterals.
Discussion: This patient had recurrent esophageal variceal hemorrhages due to NCTH, and the creation of a splenorenal shunt prevented further episodes of variceal hemorrhage. In selected patients with NCTH, especially those without sustained relief from endoscopic management and unable to tolerate pharmacologic therapy, surgical shunt should be considered earlier in the treatment course after weighing the risks of an invasive surgery versus the risk of recurrent and life-threatening variceal hemorrhage.
Disclosures:
Kim Minh Le, DO1, Amar Gupta, MD2, Raja K. Dhanekula, MS, MD, MBBS3. P4721 - Complicated Portal Vein Thrombosis Requiring Creation of a Surgical Shunt, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Kim Minh Le, DO1, Amar Gupta, MD2, Raja K. Dhanekula, MS, MD, MBBS3
1Baylor Scott & White Medical Center, Austin, TX; 2Baylor Scott & White Medical Center, Dallas, TX; 3Baylor Scott and White Round Rock, Round Rock, TX
Introduction: Portal vein thrombosis (PVT) is an uncommon condition with a prevalence of 0.7 to 1 per 100,000. Cavernous transformation of the portal vein (CTPV) is a complication of chronic PVT. The literature regarding CTPV is minimal, as most data is based on clinical series and case reports. We present a case of idiopathic PVT with CTPV complicated by non-cirrhotic portal hypertension (NCPH) manifested by recurrent esophageal variceal bleeding necessitating a surgical creation of a splenorenal shunt.
Case Description/Methods: The patient is a 37-year-old male who presented with easy bruising and was diagnosed with a PVT with CTPV. Despite preserved hepatic function, he had recurrent symptomatic anemia and melena for which he underwent four esophagogastroduodenoscopies, most revealing esophageal varices with high-risk stigmata requiring esophageal variceal ligations. He underwent a trial of non-selective beta blockers for secondary prophylaxis but unfortunately developed symptomatic hypotension. He was thus referred to transplant surgery for creation of a surgical shunt. Intraoperatively, the pressures in the splenic, superior mesenteric, and portal veins were 22 mmHg. A mesorectum shunt using the internal jugular vein was attempted to decompress the right sided portal hypertension but was unsuccessful. A splenorenal shunt was then created, decompressing both the left and right side of the spleno-mesenteric system. Pressures in the splenic vein and superior mesenteric vein dropped to 16 mmHg. The pressure in the left renal vein was 12 mmHg. This 4 mmHg porto-systemic gradient was expected to prevent bleeding from varices. Post-operative imaging showed a decrease in the upper abdominal varices and collateral vessels and near resolution of splenomegaly (15 cm to 12.5cm) and thrombocytopenia (58,000 to 132,000). There was evidence of a new thrombus within a collateral vessel near the pancreatic head, which supports functionality of the splenorenal shunt decreasing flow through the collaterals.
Discussion: This patient had recurrent esophageal variceal hemorrhages due to NCTH, and the creation of a splenorenal shunt prevented further episodes of variceal hemorrhage. In selected patients with NCTH, especially those without sustained relief from endoscopic management and unable to tolerate pharmacologic therapy, surgical shunt should be considered earlier in the treatment course after weighing the risks of an invasive surgery versus the risk of recurrent and life-threatening variceal hemorrhage.
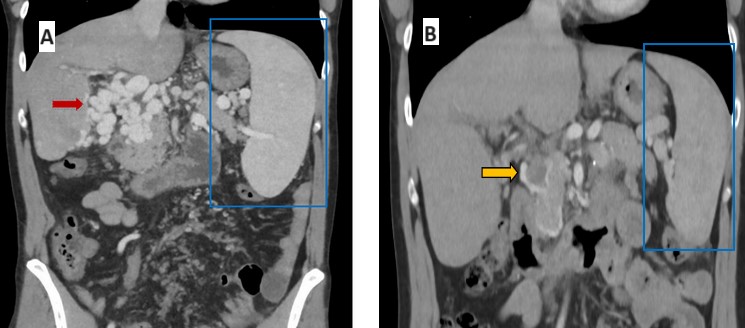
Figure: Image A shows multiple collateral vessels associated with cavernous transformation of the portal vein (red arrow) and marked splenomegaly (blue box). Image B shows the decreased size of collateral vessels, improvement in the splenomegaly (blue box), and a new thrombus within a collateral vessel (orange arrow).
Disclosures:
Kim Minh Le indicated no relevant financial relationships.
Amar Gupta indicated no relevant financial relationships.
Raja Dhanekula indicated no relevant financial relationships.
Kim Minh Le, DO1, Amar Gupta, MD2, Raja K. Dhanekula, MS, MD, MBBS3. P4721 - Complicated Portal Vein Thrombosis Requiring Creation of a Surgical Shunt, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

