Tuesday Poster Session
Category: Liver
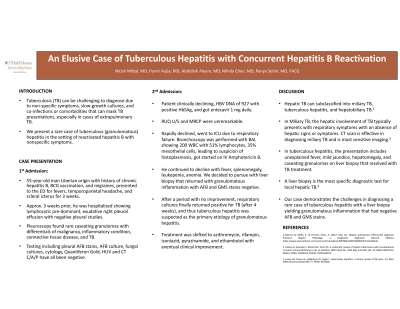
P4732 - An Elusive Case of Tuberculous Hepatitis With Concurrent Hepatitis B Reactivation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NM
Nitish Mittal, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Nitish Mittal, MD1, Parvir Aujla, MD1, Abdullah S. Aleem, MD2, Mindy Chen, MD2, Ranya Selim, MD2
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas at Houston, Houston, TX
Introduction: Tuberculosis (TB) can be challenging to diagnose due to non-specific symptoms, slow-growing cultures, and coinfections or comorbidities that can mask TB presentations, especially in cases of extrapulmonary TB involving other organs. In this case report, we present a rare case of tuberculosis (granulomatous) hepatitis with nonspecific symptoms and negative tuberculosis testing.
Case Description/Methods: A 55-year-old-male with chronic HBV, BCG vaccination, and migraines presented to the ED for fevers, headache, and scleral icterus for 3 weeks duration. Three weeks prior, he had been hospitalized for lymphocytic predominant, exudative right pleural effusion, with negative pleural studies. Pleuroscopy found rare caseating granulomas with differentials of malignancy, inflammatory condition, connective tissue disease, and TB. Testing including pleural AFB stains, AFB culture, fungal cultures, cytology, QuantiFERON gold, HIV, and CT chest/abdomen/pelvis have all been negative.
While in the ED, he was found to have elevated liver enzymes, and Mycobacterium tuberculosis PCR testing returned negative. Viral hepatitis workup showed elevated HBV DNA of 927 with positive HbSAg, and entecavir 1 mg daily was started. Right upper quadrant ultrasound and MRCP showed no remarkable findings. His liver function tests continued to uptrend, and thus a liver biopsy was pursued which showed granulomatous inflammation with AFB and GMS stains showing negative findings. Throughout his hospital course, he was transferred to ICU due to respiratory failure. Bronchoscopy with BAL showed 200 WBC, 51% lymphocytes, 35% mesothelial cells, leading to a suspicion of histoplasmosis, and intravenous amphotericin B was started. He continued to decline with fevers, splenomegaly, leukopenia, and anemia. After a period with no improvement, Karius testing and respiratory cultures finally returned with positive TB findings, and thus tuberculous hepatitis was suspected as the primary etiology of granulomatous hepatitis. Treatment was shifted to azithromycin, rifampin, isoniazid, pyrazinamide, and ethambutol with eventual clinical improvement.
Discussion: Our case demonstrates the challenges in diagnosing a rare case of tuberculous hepatitis with a liver biopsy yielding granulomatous inflammation. Although differentials for granulomatous inflammation can be broad, our case report hopes to aid clinicians in considering anti-TB treatments if other treatment protocols have failed to show clinical improvement.
Disclosures:
Nitish Mittal, MD1, Parvir Aujla, MD1, Abdullah S. Aleem, MD2, Mindy Chen, MD2, Ranya Selim, MD2. P4732 - An Elusive Case of Tuberculous Hepatitis With Concurrent Hepatitis B Reactivation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas at Houston, Houston, TX
Introduction: Tuberculosis (TB) can be challenging to diagnose due to non-specific symptoms, slow-growing cultures, and coinfections or comorbidities that can mask TB presentations, especially in cases of extrapulmonary TB involving other organs. In this case report, we present a rare case of tuberculosis (granulomatous) hepatitis with nonspecific symptoms and negative tuberculosis testing.
Case Description/Methods: A 55-year-old-male with chronic HBV, BCG vaccination, and migraines presented to the ED for fevers, headache, and scleral icterus for 3 weeks duration. Three weeks prior, he had been hospitalized for lymphocytic predominant, exudative right pleural effusion, with negative pleural studies. Pleuroscopy found rare caseating granulomas with differentials of malignancy, inflammatory condition, connective tissue disease, and TB. Testing including pleural AFB stains, AFB culture, fungal cultures, cytology, QuantiFERON gold, HIV, and CT chest/abdomen/pelvis have all been negative.
While in the ED, he was found to have elevated liver enzymes, and Mycobacterium tuberculosis PCR testing returned negative. Viral hepatitis workup showed elevated HBV DNA of 927 with positive HbSAg, and entecavir 1 mg daily was started. Right upper quadrant ultrasound and MRCP showed no remarkable findings. His liver function tests continued to uptrend, and thus a liver biopsy was pursued which showed granulomatous inflammation with AFB and GMS stains showing negative findings. Throughout his hospital course, he was transferred to ICU due to respiratory failure. Bronchoscopy with BAL showed 200 WBC, 51% lymphocytes, 35% mesothelial cells, leading to a suspicion of histoplasmosis, and intravenous amphotericin B was started. He continued to decline with fevers, splenomegaly, leukopenia, and anemia. After a period with no improvement, Karius testing and respiratory cultures finally returned with positive TB findings, and thus tuberculous hepatitis was suspected as the primary etiology of granulomatous hepatitis. Treatment was shifted to azithromycin, rifampin, isoniazid, pyrazinamide, and ethambutol with eventual clinical improvement.
Discussion: Our case demonstrates the challenges in diagnosing a rare case of tuberculous hepatitis with a liver biopsy yielding granulomatous inflammation. Although differentials for granulomatous inflammation can be broad, our case report hopes to aid clinicians in considering anti-TB treatments if other treatment protocols have failed to show clinical improvement.
Disclosures:
Nitish Mittal indicated no relevant financial relationships.
Parvir Aujla indicated no relevant financial relationships.
Abdullah Aleem indicated no relevant financial relationships.
Mindy Chen indicated no relevant financial relationships.
Ranya Selim indicated no relevant financial relationships.
Nitish Mittal, MD1, Parvir Aujla, MD1, Abdullah S. Aleem, MD2, Mindy Chen, MD2, Ranya Selim, MD2. P4732 - An Elusive Case of Tuberculous Hepatitis With Concurrent Hepatitis B Reactivation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
