Tuesday Poster Session
Category: Liver
P4746 - In Dire Need of A-Cyst-Ance
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rumzah Paracha, MD
Yale New Haven Health
New Haven, CT
Presenting Author(s)
Rumzah Paracha, MD1, Mohammed Al-Zakwani, MD, MS2, Gabriel Heymann, MD, PhD3
1Yale New Haven Health, New Haven, CT; 2Yale New Haven Hospital, New Haven, CT; 3Yale New Haven Health, Bridgeport Hospital, New Haven, CT
Introduction: Polycystic Liver Disease (PLD) is a rare condition that typically presents in isolation as autosomal dominant polycystic liver disease or in conjunction with polycystic kidney disease. It is generally asymptomatic, however advanced disease can lead to abdominal pain, distension, obstruction, and malnutrition. We present a case of PLD causing obstructive jaundice and progressive liver injury.
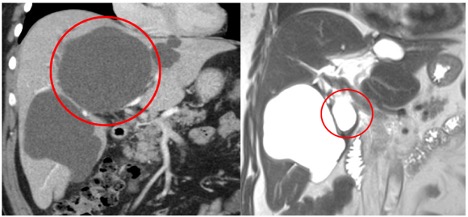
Case Description/Methods: A 60-year-old male with an unremarkable personal or family medical history presented with painless jaundice and abnormal liver chemistries. On arrival he was afebrile and hemodynamically stable. Labs were significant for total bilirubin 6.4 mg/dl, direct bilirubin 4.9 mg/dl, ALP 400 U/L, ALT 198 U/L, AST 125 U/L. A RUQ U/S showed multiple liver cysts with distal intrahepatic biliary duct dilation. A follow up CT Abdomen/Pelvis showed multiple lobulated cysts in the liver, the largest measuring 11.7 x 11.0 x 11.4 cm, and normal kidneys. This cyst was exerting mass effect, leading to displacement of portal veins and compression of the biliary tree, with resultant biliary ductal dilation. Interventional Radiology was consulted and the patient underwent drain placement into the largest cyst. Follow up MRI of the abdomen showed subsequent collapse of the cyst. The patient’s liver indices improved after drain placement, with ALP 346 and total bilirubin 4.0. He was discharged with the drain in place and plan for more definitive surgical treatment outpatient. Most recent lab results, approximately 3 weeks post-drain placement, showed continued improvement with a reduction in ALP to 176 U/L and normalization of total bilirubin at 0.9 mg/dl.
Discussion: PLD is a rare condition that can become symptomatic and have significant clinical sequelae when the cysts enlarge sufficiently to affect adjacent structures, commonly leading to abdominal distension and pain. Rarely, it can cause compression of the biliary tree leading to jaundice and pruritus, typically requiring surgical intervention. Current surgical options include fenestration, sclerotherapy, hepatectomy, and liver transplant in severe cases. Percutaneous drainage can be utilized as a temporizing measure while more definite therapies are being considered.
Additionally, PLD should be considered when encountering a patient with jaundice of unclear etiology and multiple liver cysts. This is especially important given its association with ADPKD, which has an increased risk of developing brain aneurysms, with a high mortality rate if ruptured.
Disclosures:
Rumzah Paracha, MD1, Mohammed Al-Zakwani, MD, MS2, Gabriel Heymann, MD, PhD3. P4746 - In Dire Need of A-Cyst-Ance, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Yale New Haven Health, New Haven, CT; 2Yale New Haven Hospital, New Haven, CT; 3Yale New Haven Health, Bridgeport Hospital, New Haven, CT
Introduction: Polycystic Liver Disease (PLD) is a rare condition that typically presents in isolation as autosomal dominant polycystic liver disease or in conjunction with polycystic kidney disease. It is generally asymptomatic, however advanced disease can lead to abdominal pain, distension, obstruction, and malnutrition. We present a case of PLD causing obstructive jaundice and progressive liver injury.
Case Description/Methods: A 60-year-old male with an unremarkable personal or family medical history presented with painless jaundice and abnormal liver chemistries. On arrival he was afebrile and hemodynamically stable. Labs were significant for total bilirubin 6.4 mg/dl, direct bilirubin 4.9 mg/dl, ALP 400 U/L, ALT 198 U/L, AST 125 U/L. A RUQ U/S showed multiple liver cysts with distal intrahepatic biliary duct dilation. A follow up CT Abdomen/Pelvis showed multiple lobulated cysts in the liver, the largest measuring 11.7 x 11.0 x 11.4 cm, and normal kidneys. This cyst was exerting mass effect, leading to displacement of portal veins and compression of the biliary tree, with resultant biliary ductal dilation. Interventional Radiology was consulted and the patient underwent drain placement into the largest cyst. Follow up MRI of the abdomen showed subsequent collapse of the cyst. The patient’s liver indices improved after drain placement, with ALP 346 and total bilirubin 4.0. He was discharged with the drain in place and plan for more definitive surgical treatment outpatient. Most recent lab results, approximately 3 weeks post-drain placement, showed continued improvement with a reduction in ALP to 176 U/L and normalization of total bilirubin at 0.9 mg/dl.
Discussion: PLD is a rare condition that can become symptomatic and have significant clinical sequelae when the cysts enlarge sufficiently to affect adjacent structures, commonly leading to abdominal distension and pain. Rarely, it can cause compression of the biliary tree leading to jaundice and pruritus, typically requiring surgical intervention. Current surgical options include fenestration, sclerotherapy, hepatectomy, and liver transplant in severe cases. Percutaneous drainage can be utilized as a temporizing measure while more definite therapies are being considered.
Additionally, PLD should be considered when encountering a patient with jaundice of unclear etiology and multiple liver cysts. This is especially important given its association with ADPKD, which has an increased risk of developing brain aneurysms, with a high mortality rate if ruptured.
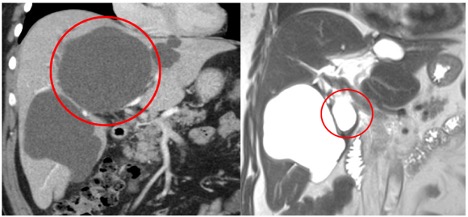
Figure: Figure 1: CT Abdomen/Pelvis w IV contrast demonstrating multiple hepatic cysts, the largest at 11.7 x 11.0 x 11.4 cm circled (left). MRI Abdomen with IV contrast demonstrating collapse of the pre-existing cyst, circled, after drain placement (right).
Disclosures:
Rumzah Paracha indicated no relevant financial relationships.
Mohammed Al-Zakwani indicated no relevant financial relationships.
Gabriel Heymann indicated no relevant financial relationships.
Rumzah Paracha, MD1, Mohammed Al-Zakwani, MD, MS2, Gabriel Heymann, MD, PhD3. P4746 - In Dire Need of A-Cyst-Ance, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

