Tuesday Poster Session
Category: Liver
P4773 - From Fever to Hepatectomy: Diagnosing and Managing Secondary Sclerosing Cholangitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Adedamola O. Bello, MD
University of Saskatchewan
Saskatoon, SK, Canada
Presenting Author(s)
Adedamola O. Bello, MD, Tom Guzowski, MD
University of Saskatchewan, Saskatoon, SK, Canada
Introduction: Cholecystectomy, a common surgical procedure, is generally safe with a low complication rate. However, a small subset of patients may develop complex postoperative issues, including sclerosing cholangitis. This chronic disease, marked by inflammation and narrowing of the bile ducts, can be caused by surgical trauma. Although rare, post-cholecystectomy sclerosing cholangitis can lead to severe biliary and liver problems, including recurrent cholangitis and liver abscesses, posing significant management challenges.
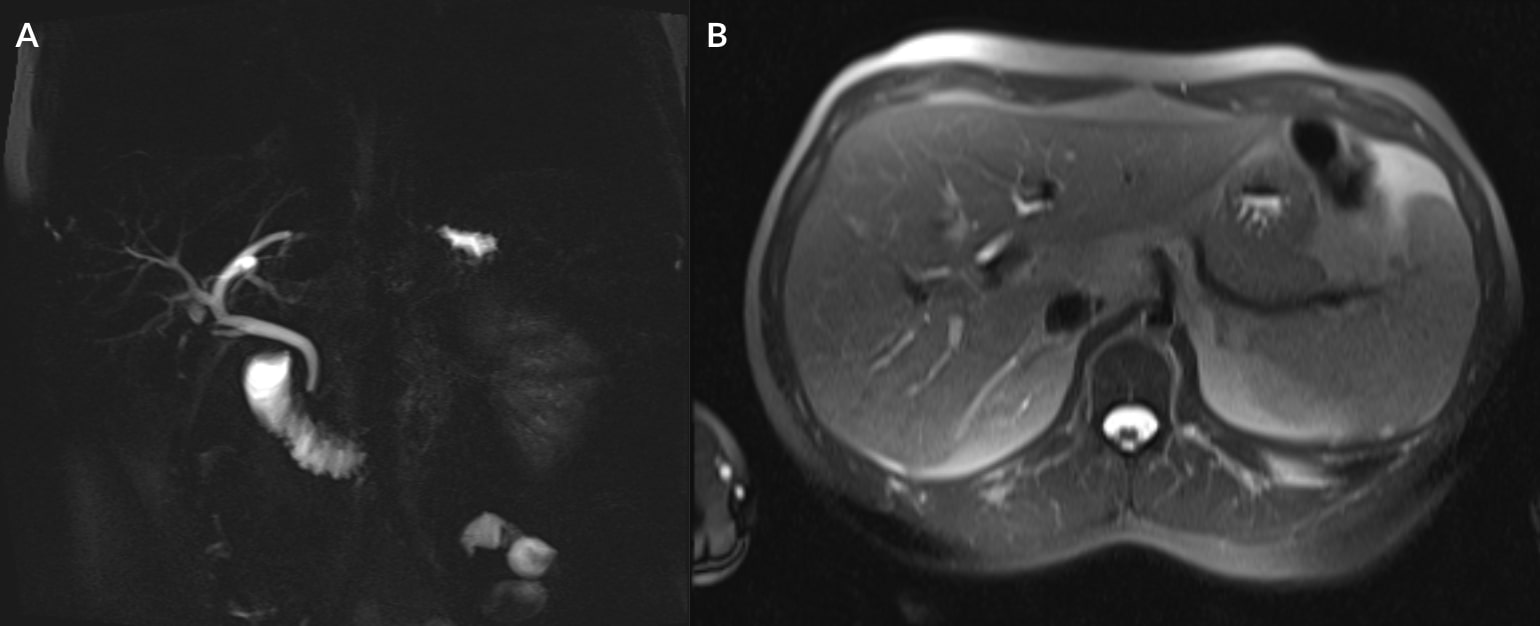
Case Description/Methods: This report details a challenging case of fever of unknown origin following a cholecystectomy in a middle-aged male with a history of choledocholithiasis. In addition to his persistent fever, he experienced a constellation of nonspecific symptoms including anorexia, abdominal pain, chronic nausea, dyspepsia, and significant weight loss post-cholecystectomy. Initial investigations included blood cultures, serologic tests for infectious and rheumatologic markers, pan-endoscopy and imaging studies; however these investigations were inconclusive. Gastroscopy and CT scans revealed nonspecific findings, such as mild erosive gastritis and ill-defined low-density areas in liver segments. MRI/MRCP played a crucial role in elucidating the diagnosis, revealing intrahepatic duct dilatation and T2 signal debris suggestive of biliary obstruction and possible infection. Percutaneous drainage yielded pus cultured as methicillin-sensitive Staphylococcus aureus and antibiotics were initiated. However due to persistent fever and complex intrahepatic duct alterations, the definitive treatment was a subsequent segmental hepatectomy. The histopathological findings suggested secondary sclerosing cholangitis with a resulting liver abscess that was not easy to visualize on initial imaging.
Discussion: This case underscores the importance of considering post-cholecystectomy secondary sclerosing cholangitis in the differential diagnosis of fever of unknown origin, particularly when accompanied by hepatobiliary abnormalities. It also emphasizes the need for a thorough diagnostic workup, the challenges in differential diagnosis, and the importance of a tailored management plan to ensure timely and appropriate interventions.
Disclosures:
Adedamola O. Bello, MD, Tom Guzowski, MD. P4773 - From Fever to Hepatectomy: Diagnosing and Managing Secondary Sclerosing Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Saskatchewan, Saskatoon, SK, Canada
Introduction: Cholecystectomy, a common surgical procedure, is generally safe with a low complication rate. However, a small subset of patients may develop complex postoperative issues, including sclerosing cholangitis. This chronic disease, marked by inflammation and narrowing of the bile ducts, can be caused by surgical trauma. Although rare, post-cholecystectomy sclerosing cholangitis can lead to severe biliary and liver problems, including recurrent cholangitis and liver abscesses, posing significant management challenges.
Case Description/Methods: This report details a challenging case of fever of unknown origin following a cholecystectomy in a middle-aged male with a history of choledocholithiasis. In addition to his persistent fever, he experienced a constellation of nonspecific symptoms including anorexia, abdominal pain, chronic nausea, dyspepsia, and significant weight loss post-cholecystectomy. Initial investigations included blood cultures, serologic tests for infectious and rheumatologic markers, pan-endoscopy and imaging studies; however these investigations were inconclusive. Gastroscopy and CT scans revealed nonspecific findings, such as mild erosive gastritis and ill-defined low-density areas in liver segments. MRI/MRCP played a crucial role in elucidating the diagnosis, revealing intrahepatic duct dilatation and T2 signal debris suggestive of biliary obstruction and possible infection. Percutaneous drainage yielded pus cultured as methicillin-sensitive Staphylococcus aureus and antibiotics were initiated. However due to persistent fever and complex intrahepatic duct alterations, the definitive treatment was a subsequent segmental hepatectomy. The histopathological findings suggested secondary sclerosing cholangitis with a resulting liver abscess that was not easy to visualize on initial imaging.
Discussion: This case underscores the importance of considering post-cholecystectomy secondary sclerosing cholangitis in the differential diagnosis of fever of unknown origin, particularly when accompanied by hepatobiliary abnormalities. It also emphasizes the need for a thorough diagnostic workup, the challenges in differential diagnosis, and the importance of a tailored management plan to ensure timely and appropriate interventions.
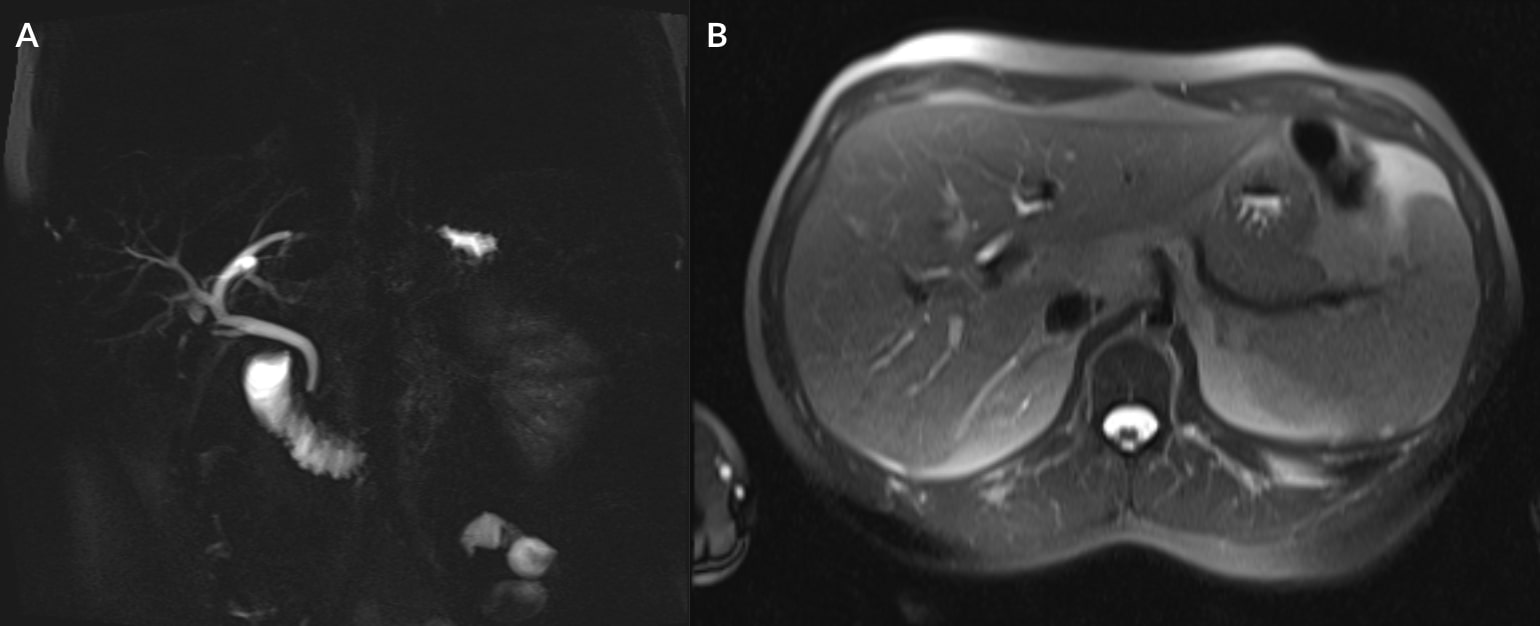
Figure: Fig. 1 A) MRCP, B) MRI
Intrahepatic duct dilatation in the right hepatic lobe. No obstructing mass is identified. Debris noted within the ducts and heterogeneous enhancement of the surrounding liver parenchyma.
Intrahepatic duct dilatation in the right hepatic lobe. No obstructing mass is identified. Debris noted within the ducts and heterogeneous enhancement of the surrounding liver parenchyma.
Disclosures:
Adedamola Bello indicated no relevant financial relationships.
Tom Guzowski indicated no relevant financial relationships.
Adedamola O. Bello, MD, Tom Guzowski, MD. P4773 - From Fever to Hepatectomy: Diagnosing and Managing Secondary Sclerosing Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
