Tuesday Poster Session
Category: Liver
P4782 - Cholangioblastic Variant of Intrahepatic Cholangiocarcinoma in a 33-Year-Old Female
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Elise Roman, MD
University Hospitals Cleveland Medical Center
Bay Village, OH
Presenting Author(s)
Elise Roman, MD1, Rebecca Obeng, MD, PhD, MPH1, Naemat Sandhu, MD2
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: The cholangioblastic variant of intrahepatic cholangiocarcinoma (CCAi) is an exceedingly rare biliary tract malignancy. Here we review a case of this variant incidentally discovered in a 33-year-old female.
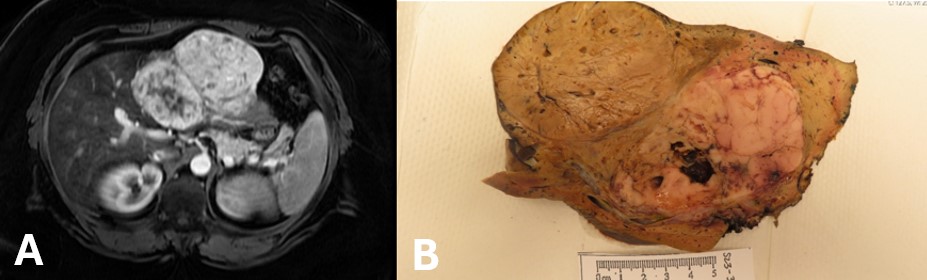
Case Description/Methods: A 33-year-old female presented to the emergency department with left lower abdominal pain. CT abdomen revealed a well-marginated, 12-cm left hepatic lobe mass. Liver function labs were normal. A subsequent MRI showed a large conglomerate of enhancing lesions with central necrosis (Image A). Differential included multiple adjacent hepatic adenomas, adjacent giant cavernous hemangiomas, or fibrolamellar carcinoma. Because of a BMI over 70, she was too high risk for hepatectomy, thus she underwent a roux-en-Y gastric bypass.
Hepatectomy was performed one year later once adequate weight loss was achieved. Initial pathology revealed a multifocal intrahepatic neoplasm, with final diagnosis of cholangioblastic variant of CCAi. The explanted liver specimen showed a large, tan, exophytic mass (Image B). Histology showed tumor cells growing in solid sheets and tubules with some nodules of less differentiated growth in a macrotrabecular pattern with patchy necrotic areas. The tumor cells were positive for cytokeratin AE1/3, cam 5.2, CK7, inhibin, ALB-ISH, and synaptophysin. There was focal mucicarmine positivity and INI-1 showed retained nuclear staining. Gene fusion was unable to be performed.
The patient was started on capecitabine for six cycles. Her most recent CT showed no evidence of recurrence or metastasis.
Discussion: The cholangioblastic variant of CCAi has been reported in only 5 cases to date, with an average age of 32. Unlike typical cholangiocarcinoma, these patients did not have histories of liver disease or other known risk factors for hepatic malignancies. Trends in the pathological characterization have shown cells that stain strongly positive for inhibin, and immunohistochemistry with positive expression of CK7, CK19, synaptophysin and chromogranin, similar to neuroendocrine tumors. In recent studies a specific gene fusion (NIPBL-NACC1) was discovered as an important surrogate marker.
Patients with incidental, irregularly-appearing hepatic masses should undergo further investigation. If a neuroendocrine tumor is suspected, cholangioblastic CCAi should also be considered. It is possible that as awareness increases, previous cases of neuroendocrine tumors may be revealed to actually be cholangioblastic CCAi, helping to further identify diagnostic patterns.
Disclosures:
Elise Roman, MD1, Rebecca Obeng, MD, PhD, MPH1, Naemat Sandhu, MD2. P4782 - Cholangioblastic Variant of Intrahepatic Cholangiocarcinoma in a 33-Year-Old Female, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: The cholangioblastic variant of intrahepatic cholangiocarcinoma (CCAi) is an exceedingly rare biliary tract malignancy. Here we review a case of this variant incidentally discovered in a 33-year-old female.
Case Description/Methods: A 33-year-old female presented to the emergency department with left lower abdominal pain. CT abdomen revealed a well-marginated, 12-cm left hepatic lobe mass. Liver function labs were normal. A subsequent MRI showed a large conglomerate of enhancing lesions with central necrosis (Image A). Differential included multiple adjacent hepatic adenomas, adjacent giant cavernous hemangiomas, or fibrolamellar carcinoma. Because of a BMI over 70, she was too high risk for hepatectomy, thus she underwent a roux-en-Y gastric bypass.
Hepatectomy was performed one year later once adequate weight loss was achieved. Initial pathology revealed a multifocal intrahepatic neoplasm, with final diagnosis of cholangioblastic variant of CCAi. The explanted liver specimen showed a large, tan, exophytic mass (Image B). Histology showed tumor cells growing in solid sheets and tubules with some nodules of less differentiated growth in a macrotrabecular pattern with patchy necrotic areas. The tumor cells were positive for cytokeratin AE1/3, cam 5.2, CK7, inhibin, ALB-ISH, and synaptophysin. There was focal mucicarmine positivity and INI-1 showed retained nuclear staining. Gene fusion was unable to be performed.
The patient was started on capecitabine for six cycles. Her most recent CT showed no evidence of recurrence or metastasis.
Discussion: The cholangioblastic variant of CCAi has been reported in only 5 cases to date, with an average age of 32. Unlike typical cholangiocarcinoma, these patients did not have histories of liver disease or other known risk factors for hepatic malignancies. Trends in the pathological characterization have shown cells that stain strongly positive for inhibin, and immunohistochemistry with positive expression of CK7, CK19, synaptophysin and chromogranin, similar to neuroendocrine tumors. In recent studies a specific gene fusion (NIPBL-NACC1) was discovered as an important surrogate marker.
Patients with incidental, irregularly-appearing hepatic masses should undergo further investigation. If a neuroendocrine tumor is suspected, cholangioblastic CCAi should also be considered. It is possible that as awareness increases, previous cases of neuroendocrine tumors may be revealed to actually be cholangioblastic CCAi, helping to further identify diagnostic patterns.
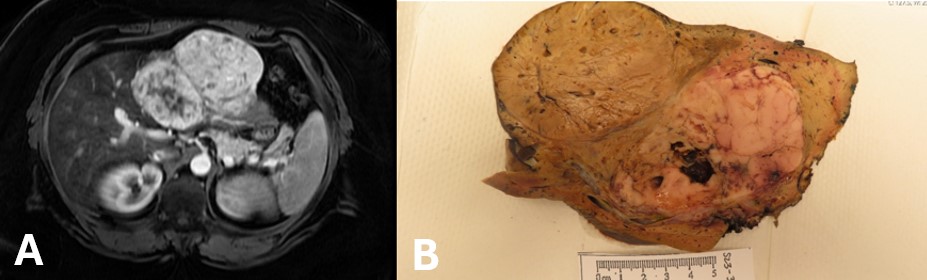
Figure: Image A. MRI showing a large conglomerate of enhancing lesions with central necrosis ; Image B. Explanted liver with a large, tan, exophytic mass.
Disclosures:
Elise Roman indicated no relevant financial relationships.
Rebecca Obeng indicated no relevant financial relationships.
Naemat Sandhu indicated no relevant financial relationships.
Elise Roman, MD1, Rebecca Obeng, MD, PhD, MPH1, Naemat Sandhu, MD2. P4782 - Cholangioblastic Variant of Intrahepatic Cholangiocarcinoma in a 33-Year-Old Female, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
