Tuesday Poster Session
Category: Liver
P4789 - Unmasking Hepatic Amyloidosis in a Patient with Recurrent Ascites
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- YW
Yael Wollstein, MD
University of Chicago Medicine
Chicago, IL
Presenting Author(s)
Yael Wollstein, MD, Sarah Park, MD, Natali Ronen, MD, Sonali Paul, MD, MSc, Alan L. Hutchison, MD, PhD
University of Chicago Medicine, Chicago, IL
Introduction: Light chain (AL) amyloidosis is a systemic disease characterized by immunoglobulin light chain deposition in organs including the liver. Variable clinical presentations and lack of specific findings associated with hepatic amyloidosis can lead to misdiagnosis or delayed identification, at times only after other organs demonstrate signs of infiltrative disease.
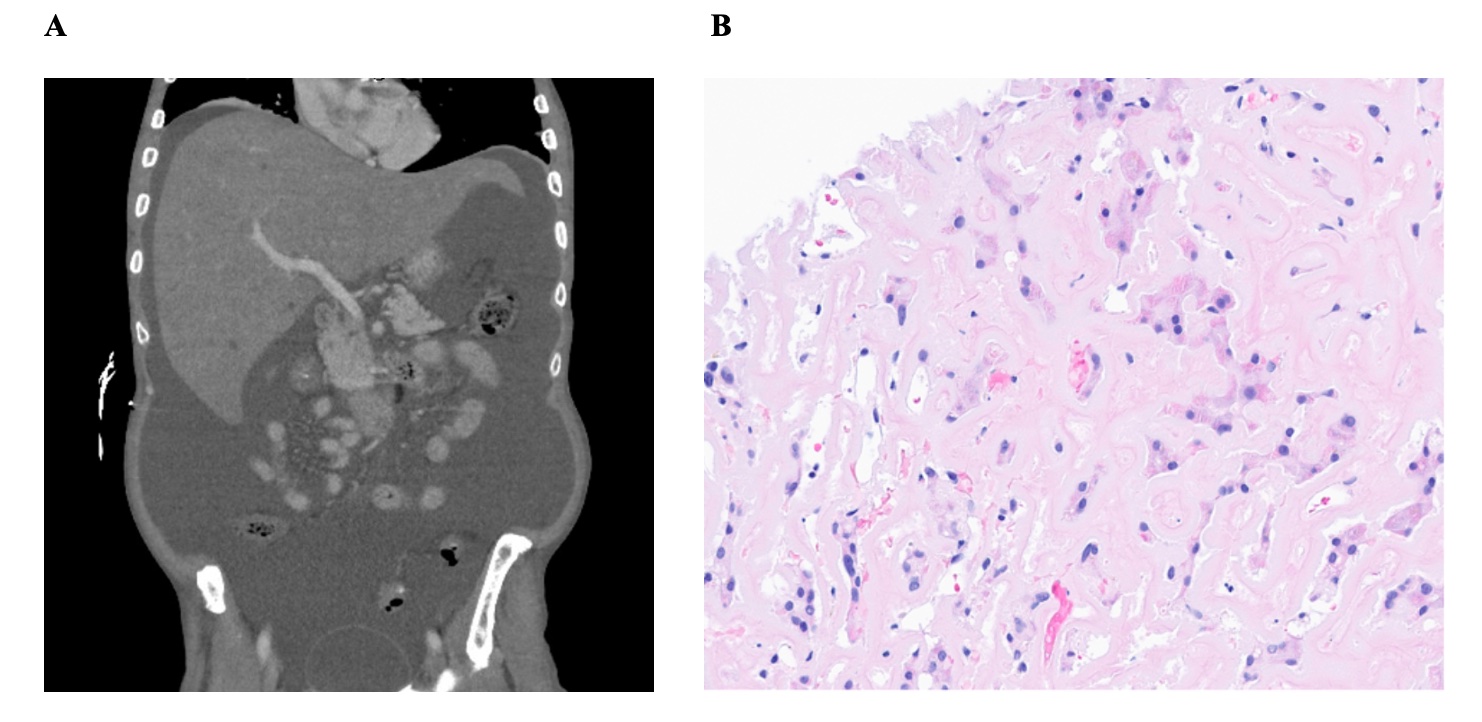
Case Description/Methods: A 67 year old man with history of hyperlipidemia, hypertension, and carpal tunnel syndrome (CTS) treated 15 years prior presented to hepatology clinic for evaluation of recurrent ascites. He had recently been admitted to another hospital, where steatosis was noted on ultrasound and attributed to MASLD. His blood pressure was 91/60 with temporal wasting, massive ascites and 1+ lower extremity edema on exam. Labs were notable for alkaline phosphatase (AP) 602, INR 1.3, Cr 1.57. An echocardiogram showed hypertrophic cardiomyopathy with septal thickening and CT showed hepatomegaly (Fig. 1A). His clinical course was complicated by hepatic encephalopathy (HE) and esophageal variceal bleed requiring banding. Given hepatic decompensation with preserved INR and proteinuria, the patient underwent liver biopsy showing extensive amyloid deposition with minimal residual markedly compressed trabecular cords of hepatocytes (Fig. 1B). Congo red stain was positive. He underwent transjugular intrahepatic portosystemic shunt (TIPS) which reduced portal pressure from 24 to 12 mmHg. He developed refractory HE which did not improve after TIPS downsizing, and his kidney function worsened. He was too frail for transplant and too decompensated for chemotherapy. He was later transitioned to comfort care and passed away.
Discussion: Elevated AP and hepatomegaly are the most common initial signs of hepatic amyloidosis (HA) but are often missed given the relative rarity of HA. Infiltrative disease should be considered in patients with these findings as well as portal hypertension and preserved INR, with biopsy needed for definitive diagnosis. Given the multisystem involvement of amyloidosis, it may first be detected via other organ manifestations, such as cardiac/renal dysfunction. Soft tissue disorders, such as CTS, can present years prior to other signs, as seen here. Though there was historical concern that biopsy or TIPS of HA could result in liver rupture, multiple reports show these procedures are safe. Treatment options include chemotherapy and stem cell transplant, though our patient was not a candidate due to frailty.
Disclosures:
Yael Wollstein, MD, Sarah Park, MD, Natali Ronen, MD, Sonali Paul, MD, MSc, Alan L. Hutchison, MD, PhD. P4789 - Unmasking Hepatic Amyloidosis in a Patient with Recurrent Ascites, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Chicago Medicine, Chicago, IL
Introduction: Light chain (AL) amyloidosis is a systemic disease characterized by immunoglobulin light chain deposition in organs including the liver. Variable clinical presentations and lack of specific findings associated with hepatic amyloidosis can lead to misdiagnosis or delayed identification, at times only after other organs demonstrate signs of infiltrative disease.
Case Description/Methods: A 67 year old man with history of hyperlipidemia, hypertension, and carpal tunnel syndrome (CTS) treated 15 years prior presented to hepatology clinic for evaluation of recurrent ascites. He had recently been admitted to another hospital, where steatosis was noted on ultrasound and attributed to MASLD. His blood pressure was 91/60 with temporal wasting, massive ascites and 1+ lower extremity edema on exam. Labs were notable for alkaline phosphatase (AP) 602, INR 1.3, Cr 1.57. An echocardiogram showed hypertrophic cardiomyopathy with septal thickening and CT showed hepatomegaly (Fig. 1A). His clinical course was complicated by hepatic encephalopathy (HE) and esophageal variceal bleed requiring banding. Given hepatic decompensation with preserved INR and proteinuria, the patient underwent liver biopsy showing extensive amyloid deposition with minimal residual markedly compressed trabecular cords of hepatocytes (Fig. 1B). Congo red stain was positive. He underwent transjugular intrahepatic portosystemic shunt (TIPS) which reduced portal pressure from 24 to 12 mmHg. He developed refractory HE which did not improve after TIPS downsizing, and his kidney function worsened. He was too frail for transplant and too decompensated for chemotherapy. He was later transitioned to comfort care and passed away.
Discussion: Elevated AP and hepatomegaly are the most common initial signs of hepatic amyloidosis (HA) but are often missed given the relative rarity of HA. Infiltrative disease should be considered in patients with these findings as well as portal hypertension and preserved INR, with biopsy needed for definitive diagnosis. Given the multisystem involvement of amyloidosis, it may first be detected via other organ manifestations, such as cardiac/renal dysfunction. Soft tissue disorders, such as CTS, can present years prior to other signs, as seen here. Though there was historical concern that biopsy or TIPS of HA could result in liver rupture, multiple reports show these procedures are safe. Treatment options include chemotherapy and stem cell transplant, though our patient was not a candidate due to frailty.
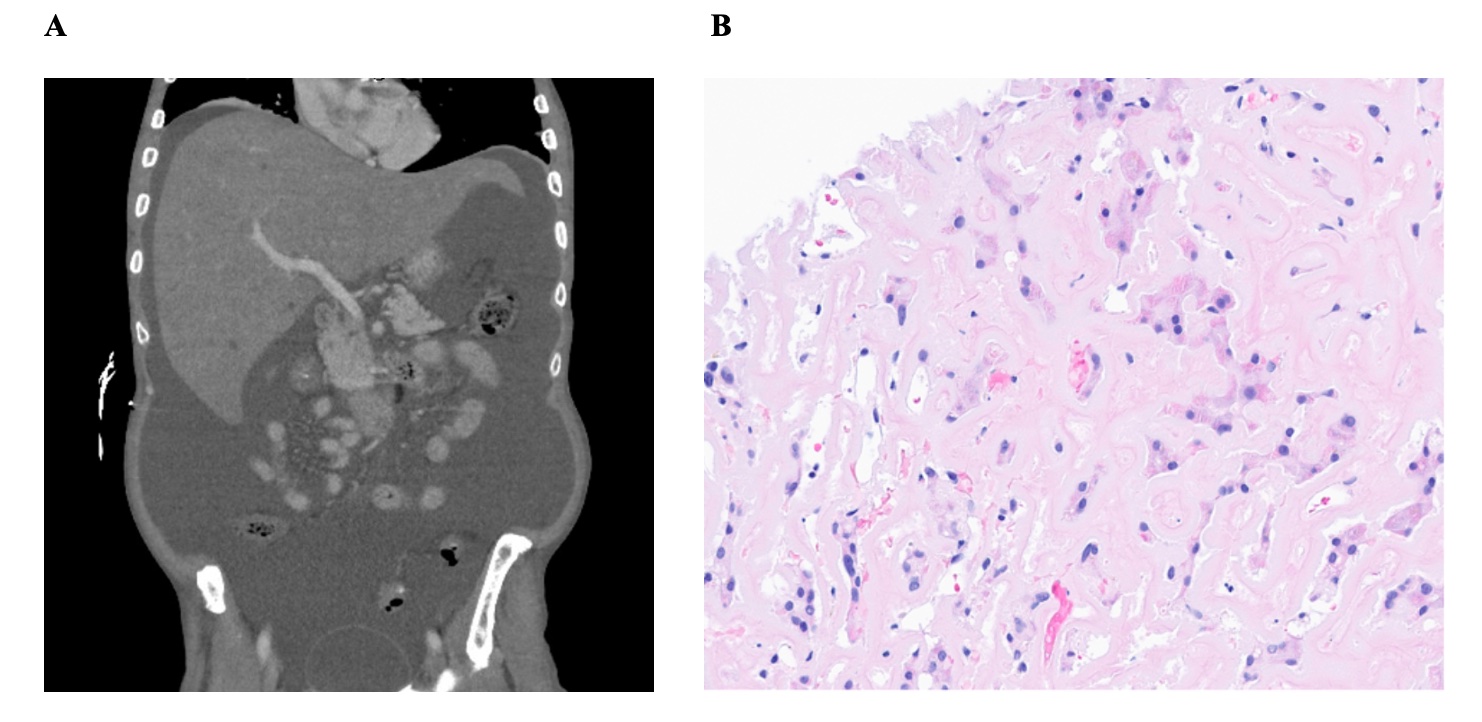
Figure: Fig. 1. A) Abdominal CT with hepatomegaly and ascites. B) Liver biopsy with scattered markedly compressed trabecular cords of hepatocytes (dark purple), clearly displaced by extensive amyloid deposition (light pink).
Disclosures:
Yael Wollstein indicated no relevant financial relationships.
Sarah Park indicated no relevant financial relationships.
Natali Ronen indicated no relevant financial relationships.
Sonali Paul: Intercept – Grant/Research Support. TARGET PharmaSolutions – Grant/Research Support.
Alan Hutchison indicated no relevant financial relationships.
Yael Wollstein, MD, Sarah Park, MD, Natali Ronen, MD, Sonali Paul, MD, MSc, Alan L. Hutchison, MD, PhD. P4789 - Unmasking Hepatic Amyloidosis in a Patient with Recurrent Ascites, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
