Tuesday Poster Session
Category: Liver
P4791 - Primary Hepatic Neuroendocrine Neoplasm: A Rare Entity with a Challenging Presentation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Malek Ayoub, MD
Washington University School of Medicine in St. Louis
St. Louis, MO
Presenting Author(s)
Malek Ayoub, MD, Scott R. Anderson, MD, Vinathi Polamraju, MD, Pooja Navale, MBBS, MD, Nikolaos A. Trikalinos, MD
Washington University School of Medicine in St. Louis, St. Louis, MO
Introduction: Among neuroendocrine neoplasms (NENs), primary hepatic neuroendocrine neoplasms (PHNENs) are exceedingly rare. Their diagnosis is challenging and requires careful and meticulous exclusion of non-hepatic origins.
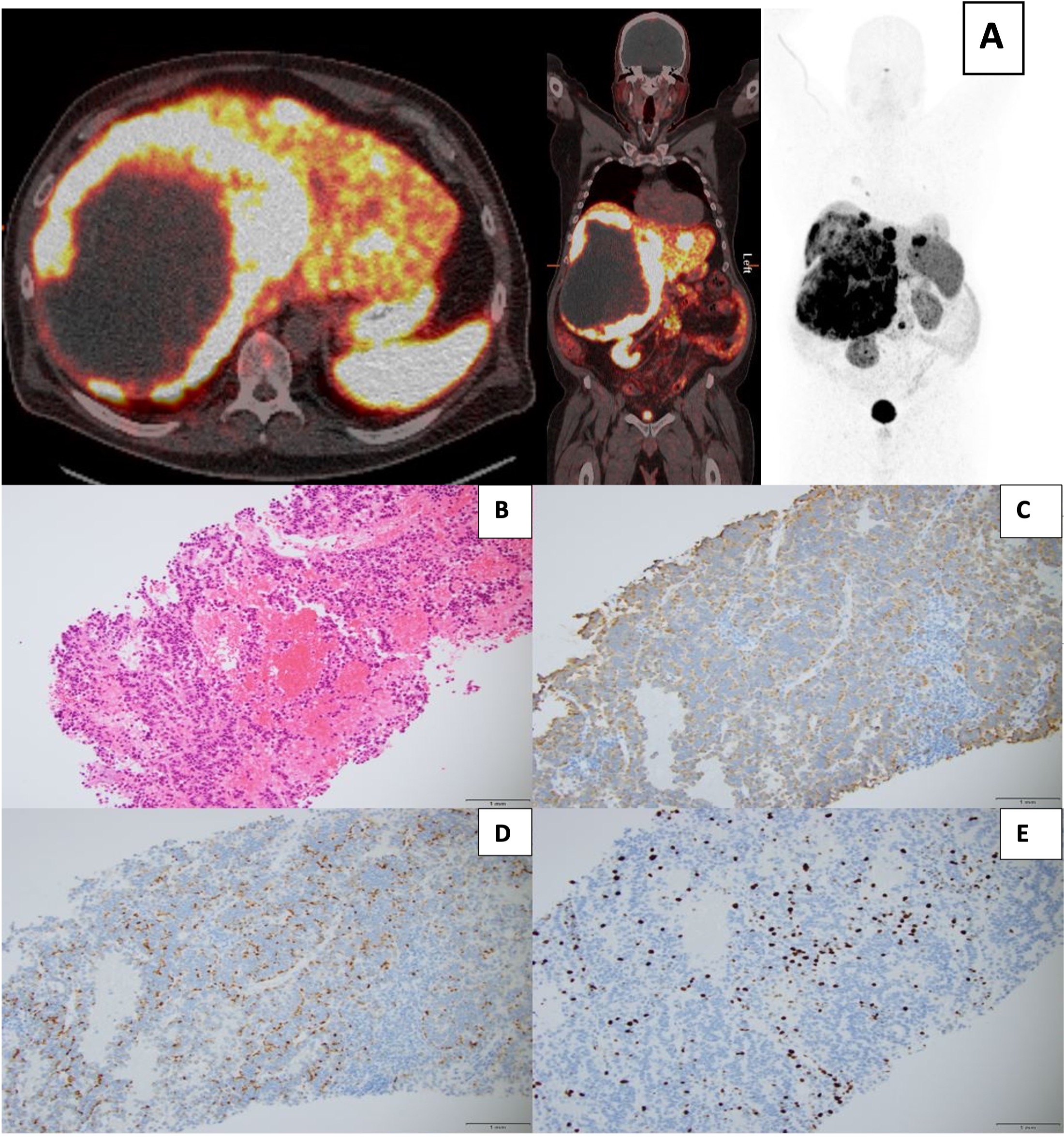
Case Description/Methods: A 63-year-old male with obesity and OSA presented with progressive dyspnea without cough and hepatomegaly, as well as elevated alkaline phosphatase level of 170 IU/L. He was treated for community acquired pneumonia with antibiotics. However, CT and MRI noted bilobar liver lesions, the largest measuring 26.3 x 21.2 x 27.2 cm, as well as upper mesenteric and periportal lymphadenopathy. While these liver lesions were nonavid on FDG PET/CT, a moderately hypermetabolic lesion in the pancreatic tail and an intensely hypermetabolic lung nodule were highlighted, suggesting metastasis from either lung or pancreas. Subsequent biopsy and histopathology of the largest liver lesion noted a well-differentiated neuroendocrine tumor (NET) with a Ki 67 index of 11% (Grade 2). Hepatocellular carcinoma was excluded given negative HepPar-1 and Arginase-1. Given neuroendocrine histology, a Dotatate PET/CT was obtained. It showed a somatostatin avid expansile, centrally photopenic but peripherally intense right hemi liver mass as well as 10 radiotracer avid satellite lesions and a periaortic lymph node (LN). Notably, no other areas were highlighted, including pancreas and the lung nodules. Given tumor multifocality, he was not a candidate for surgical intervention and was offered somatostatin analogues. To exclude primary lung cancer with liver metastasis, bronchoscopy with biopsy was pursued. Histopathology noted collections of fungal hyphae consistent with fungus ball, solidifying the diagnosis of PHNEN.
Discussion: Most malignant liver lesions are metastatic in origin, primarily from the GI or bronchopulmonary systems. Among the few primary tumors, PHNENs are exceedingly uncommon with only 151 cases described in the literature. Even after histopathologic diagnosis, advanced imaging is still necessitated as PHNEN is a diagnosis of exclusion. In our case, detailed imaging with MRI/CT, FDG and SSTR PET, and repeat biopsies were performed to confirm PHNEN with the unexpected finding of a fungal pulmonary infection.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Malek Ayoub, MD, Scott R. Anderson, MD, Vinathi Polamraju, MD, Pooja Navale, MBBS, MD, Nikolaos A. Trikalinos, MD. P4791 - Primary Hepatic Neuroendocrine Neoplasm: A Rare Entity with a Challenging Presentation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Washington University School of Medicine in St. Louis, St. Louis, MO
Introduction: Among neuroendocrine neoplasms (NENs), primary hepatic neuroendocrine neoplasms (PHNENs) are exceedingly rare. Their diagnosis is challenging and requires careful and meticulous exclusion of non-hepatic origins.
Case Description/Methods: A 63-year-old male with obesity and OSA presented with progressive dyspnea without cough and hepatomegaly, as well as elevated alkaline phosphatase level of 170 IU/L. He was treated for community acquired pneumonia with antibiotics. However, CT and MRI noted bilobar liver lesions, the largest measuring 26.3 x 21.2 x 27.2 cm, as well as upper mesenteric and periportal lymphadenopathy. While these liver lesions were nonavid on FDG PET/CT, a moderately hypermetabolic lesion in the pancreatic tail and an intensely hypermetabolic lung nodule were highlighted, suggesting metastasis from either lung or pancreas. Subsequent biopsy and histopathology of the largest liver lesion noted a well-differentiated neuroendocrine tumor (NET) with a Ki 67 index of 11% (Grade 2). Hepatocellular carcinoma was excluded given negative HepPar-1 and Arginase-1. Given neuroendocrine histology, a Dotatate PET/CT was obtained. It showed a somatostatin avid expansile, centrally photopenic but peripherally intense right hemi liver mass as well as 10 radiotracer avid satellite lesions and a periaortic lymph node (LN). Notably, no other areas were highlighted, including pancreas and the lung nodules. Given tumor multifocality, he was not a candidate for surgical intervention and was offered somatostatin analogues. To exclude primary lung cancer with liver metastasis, bronchoscopy with biopsy was pursued. Histopathology noted collections of fungal hyphae consistent with fungus ball, solidifying the diagnosis of PHNEN.
Discussion: Most malignant liver lesions are metastatic in origin, primarily from the GI or bronchopulmonary systems. Among the few primary tumors, PHNENs are exceedingly uncommon with only 151 cases described in the literature. Even after histopathologic diagnosis, advanced imaging is still necessitated as PHNEN is a diagnosis of exclusion. In our case, detailed imaging with MRI/CT, FDG and SSTR PET, and repeat biopsies were performed to confirm PHNEN with the unexpected finding of a fungal pulmonary infection.
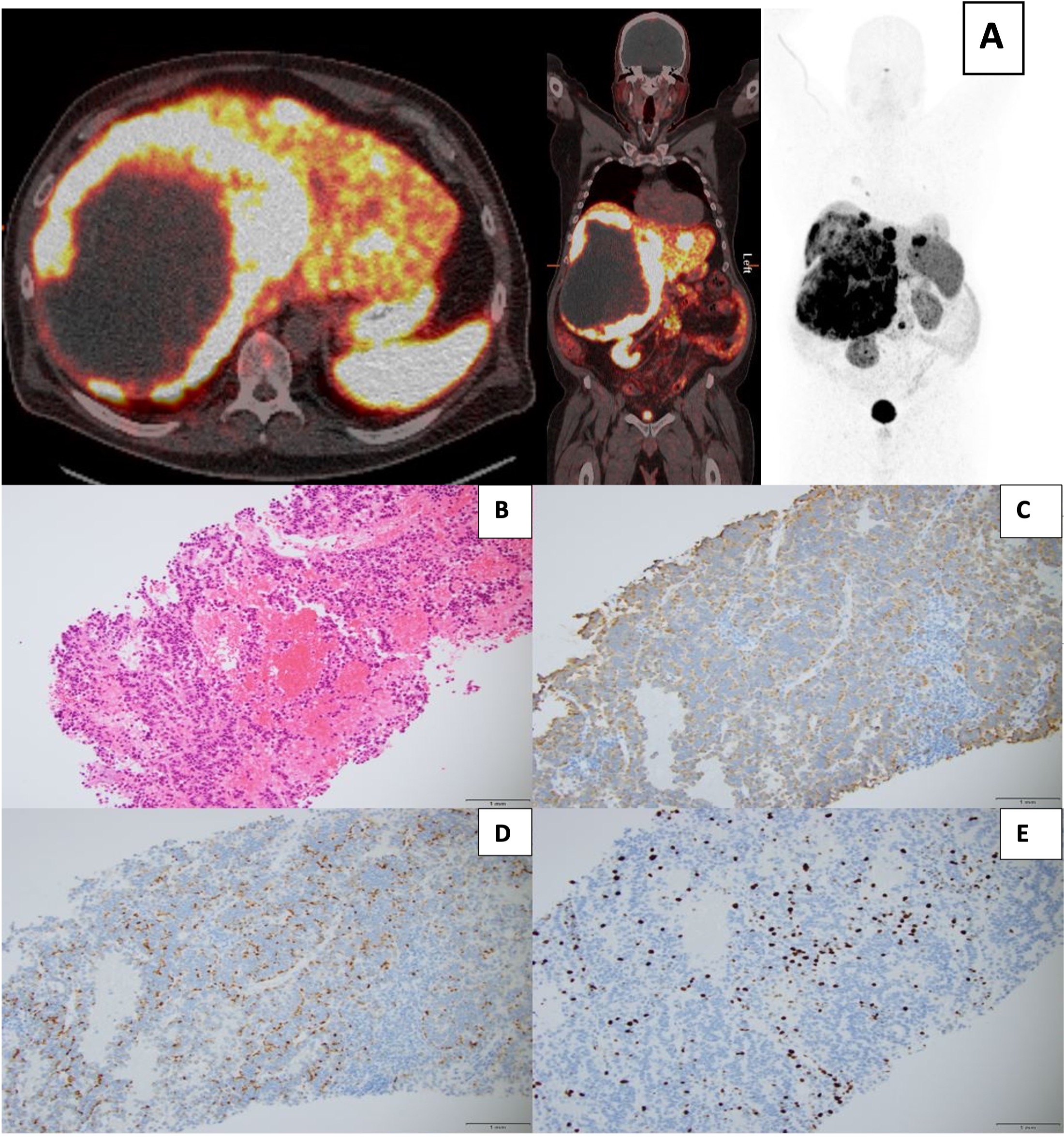
Figure: Figure 1. A) Copper 64 Dotatate PET/CT with expansile 26 cm centrally necrotic, intensely somatostatin expressing mass in the right hemiliver with at least ten satellite lesions throughout the left hemiliver. H&E stained section (B) of the liver mass demonstrating a well-differentiated neuroendocrine tumor, staining positive for synaptophysin (C) and chromogranin (D) with a Ki67 proliferation index of 11% (E).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Malek Ayoub indicated no relevant financial relationships.
Scott Anderson indicated no relevant financial relationships.
Vinathi Polamraju indicated no relevant financial relationships.
Pooja Navale indicated no relevant financial relationships.
Nikolaos Trikalinos indicated no relevant financial relationships.
Malek Ayoub, MD, Scott R. Anderson, MD, Vinathi Polamraju, MD, Pooja Navale, MBBS, MD, Nikolaos A. Trikalinos, MD. P4791 - Primary Hepatic Neuroendocrine Neoplasm: A Rare Entity with a Challenging Presentation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
