Tuesday Poster Session
Category: Liver
P4795 - Pre-Operative TIPS in a Patient With HRS and Flood Syndrome: An Alternative Approach to Management
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kristina Folta, BA
University of Washington School of Medicine
Seattle, WA
Presenting Author(s)
Kristina Folta, BA1, Sarah Gunby, MD2, Ryan Kwok, MD3, Abbey Barnard Giustini, MD, MPH3
1University of Washington School of Medicine, Seattle, WA; 2University of Washington, Seattle, WA; 3VA Puget Sound Health Care System, University of Washington, Seattle, WA
Introduction: Flood syndrome is a rare, life-threatening complication of ascites resulting in spontaneous umbilical hernia rupture. There are no practice guidelines for the management of Flood syndrome, leaving providers to manage on a case-by-case basis. This case outlines the multidisciplinary management of Flood syndrome in a patient with decompensated cirrhosis, hepatorenal syndrome (HRS) and hepatic encephalopathy (HE).
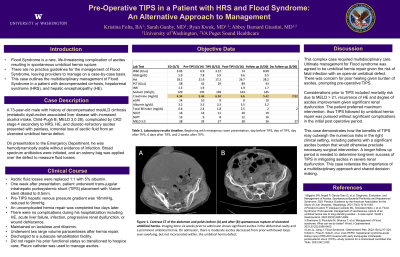
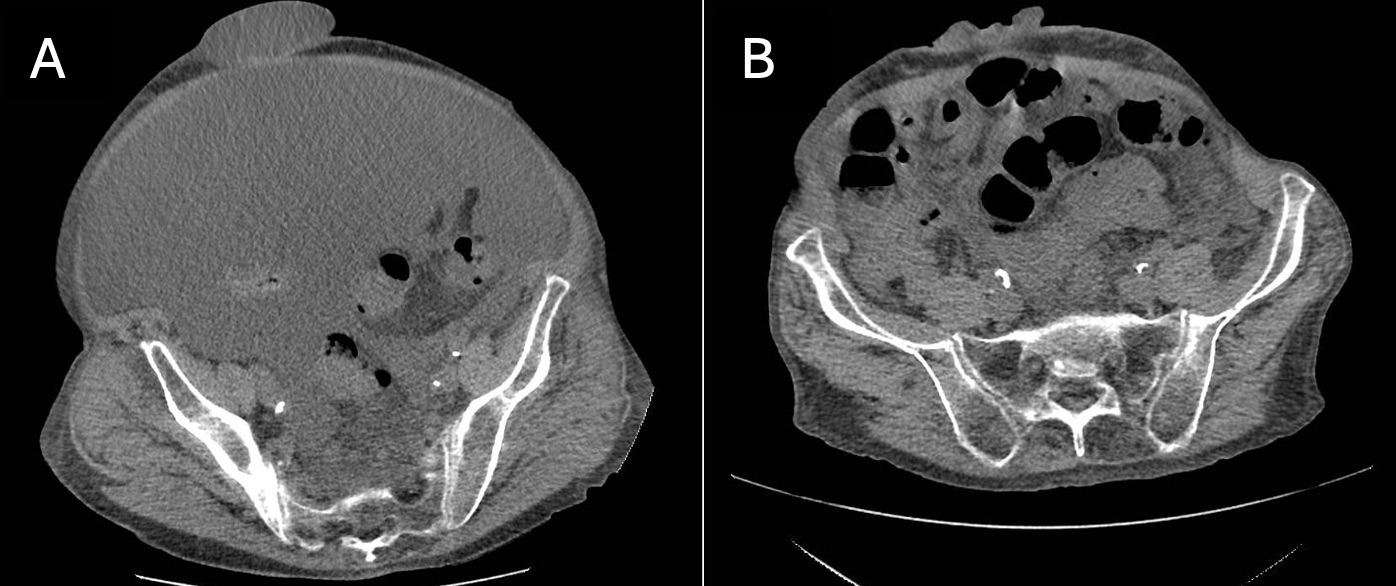
Case Description/Methods: A 73-year-old male with history of cirrhosis (Child-Pugh B, MELD 3.0 28), complicated by HRS, HE, and diuretic refractory ascites presented with painless, torrential loss of ascitic fluid from an ulcerated umbilical hernia defect. He was hemodynamically stable without evidence of infection. Laboratory studies revealed total bilirubin 0.6 and creatinine 4.34. Antibiotics were initiated and an ostomy bag was applied over the defect to measure fluid losses. Following multidisciplinary discussion, he underwent trans-jugular intrahepatic portosystemic shunt (TIPS) placement. Pre-TIPS hepatic venous pressure gradient was 18mmHg, reduced to 9mmHg. An uncomplicated hernia repair was completed two days later. He was maintained on lactulose and rifaximin. He underwent two large volume paracenteses after hernia repair. There were no significant complications post operatively. He was discharged to a subacute rehabilitation facility. Two weeks later his MELD 3.0 was 27, total bilirubin 2.0, and creatinine 2.92.
Discussion: This complex case required multidisciplinary care. Ultimate management for Flood syndrome was agreed to be umbilical hernia repair given risk of fatal infection with open-air umbilical defect. There was concern for poor healing given burden of ascites, prompting pre-operative TIPS. Considerations prior to TIPS included mortality risk due to MELD > 21, recurrence of HE, and degree of ascites improvement given significant renal dysfunction. The patient preferred maximum intervention, thus TIPS followed by umbilical hernia repair was pursued without significant complications to date.
This case demonstrates how benefits of TIPS may outweigh the numerous risks in the right clinical setting, including patients with a significant ascites burden that would otherwise preclude necessary surgical intervention. A longer follow up period is needed to determine long-term success of TIPS in mitigating ascites in severe renal dysfunction. This case reiterates the importance of a multidisciplinary approach and shared decision making.
Disclosures:
Kristina Folta, BA1, Sarah Gunby, MD2, Ryan Kwok, MD3, Abbey Barnard Giustini, MD, MPH3. P4795 - Pre-Operative TIPS in a Patient With HRS and Flood Syndrome: An Alternative Approach to Management, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Washington School of Medicine, Seattle, WA; 2University of Washington, Seattle, WA; 3VA Puget Sound Health Care System, University of Washington, Seattle, WA
Introduction: Flood syndrome is a rare, life-threatening complication of ascites resulting in spontaneous umbilical hernia rupture. There are no practice guidelines for the management of Flood syndrome, leaving providers to manage on a case-by-case basis. This case outlines the multidisciplinary management of Flood syndrome in a patient with decompensated cirrhosis, hepatorenal syndrome (HRS) and hepatic encephalopathy (HE).
Case Description/Methods: A 73-year-old male with history of cirrhosis (Child-Pugh B, MELD 3.0 28), complicated by HRS, HE, and diuretic refractory ascites presented with painless, torrential loss of ascitic fluid from an ulcerated umbilical hernia defect. He was hemodynamically stable without evidence of infection. Laboratory studies revealed total bilirubin 0.6 and creatinine 4.34. Antibiotics were initiated and an ostomy bag was applied over the defect to measure fluid losses. Following multidisciplinary discussion, he underwent trans-jugular intrahepatic portosystemic shunt (TIPS) placement. Pre-TIPS hepatic venous pressure gradient was 18mmHg, reduced to 9mmHg. An uncomplicated hernia repair was completed two days later. He was maintained on lactulose and rifaximin. He underwent two large volume paracenteses after hernia repair. There were no significant complications post operatively. He was discharged to a subacute rehabilitation facility. Two weeks later his MELD 3.0 was 27, total bilirubin 2.0, and creatinine 2.92.
Discussion: This complex case required multidisciplinary care. Ultimate management for Flood syndrome was agreed to be umbilical hernia repair given risk of fatal infection with open-air umbilical defect. There was concern for poor healing given burden of ascites, prompting pre-operative TIPS. Considerations prior to TIPS included mortality risk due to MELD > 21, recurrence of HE, and degree of ascites improvement given significant renal dysfunction. The patient preferred maximum intervention, thus TIPS followed by umbilical hernia repair was pursued without significant complications to date.
This case demonstrates how benefits of TIPS may outweigh the numerous risks in the right clinical setting, including patients with a significant ascites burden that would otherwise preclude necessary surgical intervention. A longer follow up period is needed to determine long-term success of TIPS in mitigating ascites in severe renal dysfunction. This case reiterates the importance of a multidisciplinary approach and shared decision making.
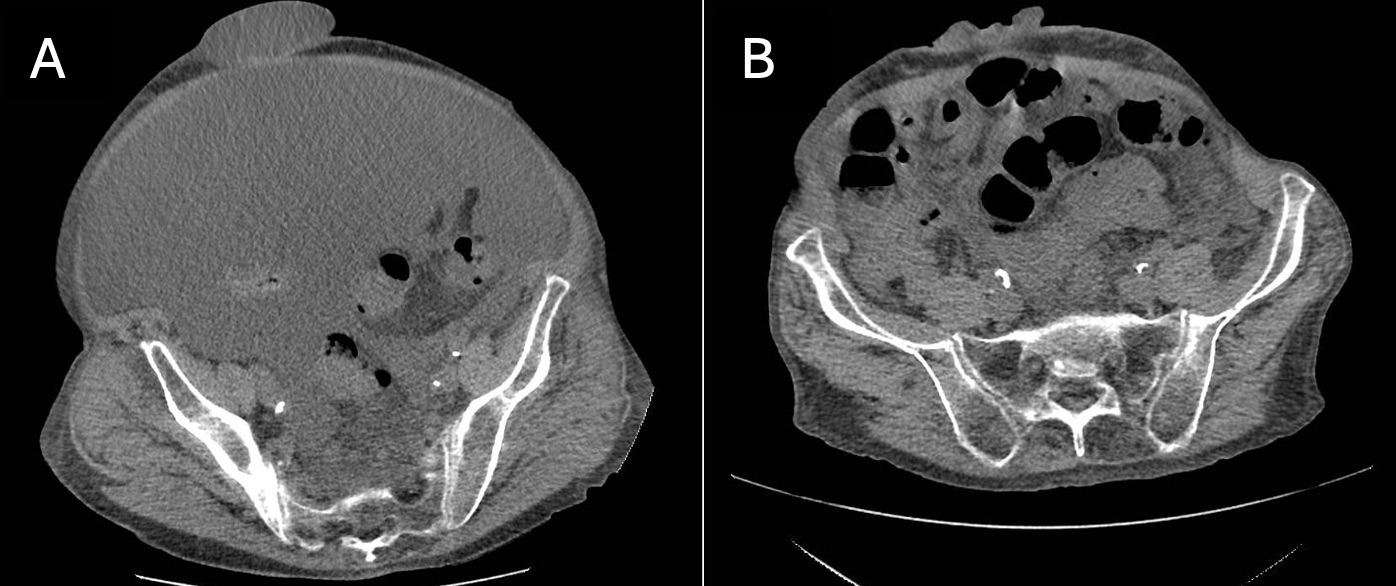
Figure: Figure 1. Contrast CT of the abdomen and pelvis before (A) and after (B) spontaneous rupture of ulcerated umbilical hernia. Imaging done six weeks prior to admission shows significant ascites in the abdominal cavity and a prominent umbilical hernia. On admission, there is moderate ascites decreased from prior with bowel loops seen overlying, but not incarcerated within, the umbilical hernia defect.
Disclosures:
Kristina Folta indicated no relevant financial relationships.
Sarah Gunby indicated no relevant financial relationships.
Ryan Kwok indicated no relevant financial relationships.
Abbey Barnard Giustini indicated no relevant financial relationships.
Kristina Folta, BA1, Sarah Gunby, MD2, Ryan Kwok, MD3, Abbey Barnard Giustini, MD, MPH3. P4795 - Pre-Operative TIPS in a Patient With HRS and Flood Syndrome: An Alternative Approach to Management, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
