Tuesday Poster Session
Category: Liver
P4803 - A Rare Drug Induced Liver Injury leading to Liver Transplantation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- PY
Pradeep Yarra, MD
Saint Louis University School of Medicine
St. Louis, MO
Presenting Author(s)
Blake Miyamoto, 1, Krishny Karunanandaa, 1, Alexander J. Thomas, MD2, Satyapriya Paritala, MD3, Pradeep Yarra, MD1, Hany Elbeshbeshy, MD4
1Saint Louis University School of Medicine, St. Louis, MO; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 4SSM Saint Louis University Hospital, St. Louis, MO
Introduction: Idiosyncratic DILI (I-DILI) is the second most common cause for Acute Liver failure (ALF) with variable latency period and poor transplant free survival rates. Losartan is an angiotensin receptor blocker used for arterial hypertension with few significant adverse effects. We present a rare case of DILI secondary to Losartan, leading to ALF needing Liver Transplantation (LT).
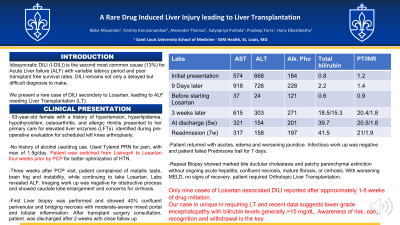
Case Description/Methods: A 63-year-old female with a history of hypertension, hyperlipidemia and osteoarthritis who was found to have abnormal liver function tests (LFTs) at pre-operative evaluation for scheduled knee arthroplasty. She complained of metallic taste, fatigue and slowing of thought process. She had no significant history of using Tylenol, herbal, non-prescribed medications, alcohol or illicit drug use. She was switched from Lisinopril to Losartan four weeks before presentation. At two weeks, with previous normal LFTs, blood work showed transaminitis (Alanine transaminase 668 IU/L, Asparate Transaminase 574 IU/L with Alkaline Phosphatase 184 IU/L) with normal synthetic function and total bilirubin (TB). In four weeks, transaminitis worsened with progressive worsening of synthetic function (Prothrombin time peak 25.1 seconds and INR 2.6) and TB at 18.5 mg/dL. Obstructive, autoimmune and genetic etiologies were ruled out. Liver biopsy showed confluent perivenular necrosis and bridging necrosis with moderate-severe mixed portal and lobular inflammation. She was treated with prednisone with minimal improvement in LFTs but worsening TB peaking at 53 mg/dl and albumin down to 1.8 mg/dL. Patient had no encephalopathy, but with no improvement in synthetic function and worsening MELD scores, we pursed repeat liver biopsy. Repeat biopsy showed marked bile ductular cholestasis, near complete or patchy parenchymal extinction with no necrosis or cirrhosis. She received Orthotopic LT and was discharged from hospital.
Discussion: Losartan rarely has been reported as a causative agent for DILI (about nine case reports), very rarely (< 0.1%), with hepatotoxicity occurring after approximately 1–8 weeks. In our report, DILI continued to ALF needing LT with no response to steroids. I-DILI is predominantly more common in women (66-71%), non-dose dependent and has dismal transplant free survival 23.5%–38.7% at 3 weeks.1 Recent data suggests lower grade encephalopathy with bilirubin levels generally >15 mg/dL.2 Liver function tests shows predominantly hepatocellular pattern of liver injury with modest alkaline phosphatase elevations
Disclosures:
Blake Miyamoto, 1, Krishny Karunanandaa, 1, Alexander J. Thomas, MD2, Satyapriya Paritala, MD3, Pradeep Yarra, MD1, Hany Elbeshbeshy, MD4. P4803 - A Rare Drug Induced Liver Injury leading to Liver Transplantation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Louis University School of Medicine, St. Louis, MO; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY; 4SSM Saint Louis University Hospital, St. Louis, MO
Introduction: Idiosyncratic DILI (I-DILI) is the second most common cause for Acute Liver failure (ALF) with variable latency period and poor transplant free survival rates. Losartan is an angiotensin receptor blocker used for arterial hypertension with few significant adverse effects. We present a rare case of DILI secondary to Losartan, leading to ALF needing Liver Transplantation (LT).
Case Description/Methods: A 63-year-old female with a history of hypertension, hyperlipidemia and osteoarthritis who was found to have abnormal liver function tests (LFTs) at pre-operative evaluation for scheduled knee arthroplasty. She complained of metallic taste, fatigue and slowing of thought process. She had no significant history of using Tylenol, herbal, non-prescribed medications, alcohol or illicit drug use. She was switched from Lisinopril to Losartan four weeks before presentation. At two weeks, with previous normal LFTs, blood work showed transaminitis (Alanine transaminase 668 IU/L, Asparate Transaminase 574 IU/L with Alkaline Phosphatase 184 IU/L) with normal synthetic function and total bilirubin (TB). In four weeks, transaminitis worsened with progressive worsening of synthetic function (Prothrombin time peak 25.1 seconds and INR 2.6) and TB at 18.5 mg/dL. Obstructive, autoimmune and genetic etiologies were ruled out. Liver biopsy showed confluent perivenular necrosis and bridging necrosis with moderate-severe mixed portal and lobular inflammation. She was treated with prednisone with minimal improvement in LFTs but worsening TB peaking at 53 mg/dl and albumin down to 1.8 mg/dL. Patient had no encephalopathy, but with no improvement in synthetic function and worsening MELD scores, we pursed repeat liver biopsy. Repeat biopsy showed marked bile ductular cholestasis, near complete or patchy parenchymal extinction with no necrosis or cirrhosis. She received Orthotopic LT and was discharged from hospital.
Discussion: Losartan rarely has been reported as a causative agent for DILI (about nine case reports), very rarely (< 0.1%), with hepatotoxicity occurring after approximately 1–8 weeks. In our report, DILI continued to ALF needing LT with no response to steroids. I-DILI is predominantly more common in women (66-71%), non-dose dependent and has dismal transplant free survival 23.5%–38.7% at 3 weeks.1 Recent data suggests lower grade encephalopathy with bilirubin levels generally >15 mg/dL.2 Liver function tests shows predominantly hepatocellular pattern of liver injury with modest alkaline phosphatase elevations
Disclosures:
Blake Miyamoto indicated no relevant financial relationships.
Krishny Karunanandaa indicated no relevant financial relationships.
Alexander Thomas indicated no relevant financial relationships.
Satyapriya Paritala indicated no relevant financial relationships.
Pradeep Yarra indicated no relevant financial relationships.
Hany Elbeshbeshy indicated no relevant financial relationships.
Blake Miyamoto, 1, Krishny Karunanandaa, 1, Alexander J. Thomas, MD2, Satyapriya Paritala, MD3, Pradeep Yarra, MD1, Hany Elbeshbeshy, MD4. P4803 - A Rare Drug Induced Liver Injury leading to Liver Transplantation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

