Tuesday Poster Session
Category: Liver
P4804 - Cholestatic Hepatitis Secondary to Bartonella henselae in a Liver Transplant Recipient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Aishwarya Thakurdesai, MBBS
University of Louisville School of Medicine
Louisville, KY
Presenting Author(s)
Aishwarya Thakurdesai, MBBS, Lucia Rivera-Matos, MD, Luis S. Marsano, MD, FACG
University of Louisville School of Medicine, Louisville, KY
Introduction: Bartonella henselae is a zoonotic pathogen whose clinical presentation depends on the patient’s immune status. While immunocompetent hosts often present with cat scratch disease, immunocompromised hosts including solid organ transplant recipients can present with other infectious syndromes. Bartonellosis is a rare infection in liver transplant recipients. We present a case of Bartonella hepatitis and sepsis in a female liver transplant recipient with prior contact with cats.
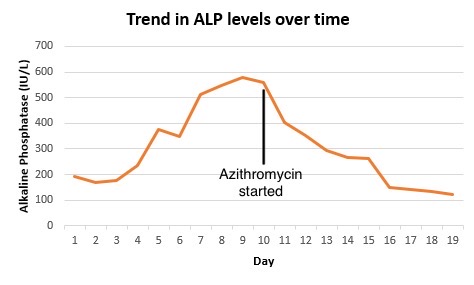
Case Description/Methods: A 41-year-old female with a history of liver transplantation for Budd-Chiari syndrome, essential thrombocythemia, chronic kidney disease, and anemia presented with worsening fatigue and exertional shortness of breath over a few weeks. Labs were remarkable for Hgb 6.7, creatinine 5.08 (baseline 2), potassium 5.4, and alkaline phosphatase (ALP) 192. Hemodialysis was initiated as her renal function did not improve with fluid resuscitation. Later, she developed fevers, chills, diarrhea, and leukocytosis. Vancomycin and Cefepime were started. Infectious workup was unrevealing other than T2 Candida PCR positive for Candida glabrata. Micafungin was added but liver function tests continued to worsen and peaked at ALP 578, AST 50, and ALT 48, INR 1.4, with a normal bilirubin. CT scan revealed possible enteritis. Duplex ultrasound of the liver was suggestive of possible recurrent cirrhosis. MRCP demonstrated no evidence of ductal dilatation or choledocholithiasis. Her fevers persisted, with procalcitonin up trending from 3.76 to 24.52 over 72 hours. Microbial cell-free DNA testing was ordered, which returned positive for Bartonella henselae species. On inquiry, the patient mentioned caring for two cats at home. Azithromycin was started resulting in resolution of fever and leukocytosis along with rapid improvement in LFTs to ALP 124, AST 35, ALT 26. The patient was discharged with plans to continue Azithromycin for 4 weeks. At 3-month follow-up, LFTs had completely normalized.
Discussion: Although a rare infection in liver transplant recipients, Bartonellosis should always be included in the differential diagnosis of patients presenting with fever, malaise, elevated ALP, lymphadenopathy, and skin lesions in the context of contact with cats. Timely diagnosis using serology, special staining, or PCR enables adequate treatment and favorable outcomes. Previous reports have shown excellent response to antibiotics like Azithromycin, Erythromycin, and Doxycycline, as corroborated by our case.
Disclosures:
Aishwarya Thakurdesai, MBBS, Lucia Rivera-Matos, MD, Luis S. Marsano, MD, FACG. P4804 - Cholestatic Hepatitis Secondary to <i>Bartonella henselae</i> in a Liver Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Louisville School of Medicine, Louisville, KY
Introduction: Bartonella henselae is a zoonotic pathogen whose clinical presentation depends on the patient’s immune status. While immunocompetent hosts often present with cat scratch disease, immunocompromised hosts including solid organ transplant recipients can present with other infectious syndromes. Bartonellosis is a rare infection in liver transplant recipients. We present a case of Bartonella hepatitis and sepsis in a female liver transplant recipient with prior contact with cats.
Case Description/Methods: A 41-year-old female with a history of liver transplantation for Budd-Chiari syndrome, essential thrombocythemia, chronic kidney disease, and anemia presented with worsening fatigue and exertional shortness of breath over a few weeks. Labs were remarkable for Hgb 6.7, creatinine 5.08 (baseline 2), potassium 5.4, and alkaline phosphatase (ALP) 192. Hemodialysis was initiated as her renal function did not improve with fluid resuscitation. Later, she developed fevers, chills, diarrhea, and leukocytosis. Vancomycin and Cefepime were started. Infectious workup was unrevealing other than T2 Candida PCR positive for Candida glabrata. Micafungin was added but liver function tests continued to worsen and peaked at ALP 578, AST 50, and ALT 48, INR 1.4, with a normal bilirubin. CT scan revealed possible enteritis. Duplex ultrasound of the liver was suggestive of possible recurrent cirrhosis. MRCP demonstrated no evidence of ductal dilatation or choledocholithiasis. Her fevers persisted, with procalcitonin up trending from 3.76 to 24.52 over 72 hours. Microbial cell-free DNA testing was ordered, which returned positive for Bartonella henselae species. On inquiry, the patient mentioned caring for two cats at home. Azithromycin was started resulting in resolution of fever and leukocytosis along with rapid improvement in LFTs to ALP 124, AST 35, ALT 26. The patient was discharged with plans to continue Azithromycin for 4 weeks. At 3-month follow-up, LFTs had completely normalized.
Discussion: Although a rare infection in liver transplant recipients, Bartonellosis should always be included in the differential diagnosis of patients presenting with fever, malaise, elevated ALP, lymphadenopathy, and skin lesions in the context of contact with cats. Timely diagnosis using serology, special staining, or PCR enables adequate treatment and favorable outcomes. Previous reports have shown excellent response to antibiotics like Azithromycin, Erythromycin, and Doxycycline, as corroborated by our case.
Figure: Figure 1: Trend in Alkaline Phosphatase levels over the hospital course. Levels began to decrease after initiation of antibiotic therapy with Azithromycin.
Disclosures:
Aishwarya Thakurdesai indicated no relevant financial relationships.
Lucia Rivera-Matos indicated no relevant financial relationships.
Luis Marsano indicated no relevant financial relationships.
Aishwarya Thakurdesai, MBBS, Lucia Rivera-Matos, MD, Luis S. Marsano, MD, FACG. P4804 - Cholestatic Hepatitis Secondary to <i>Bartonella henselae</i> in a Liver Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
