Tuesday Poster Session
Category: Liver
P4833 - Beyond Routine: Challenges in Acute Appendicitis with Gangrenous Perforation and Sepsis Complicated by Hyperbilirubinemia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sana Afreen Ansari, MD
Centinela Hospital Medical Center
Inglewood, CA
Presenting Author(s)
Nikitha Chellapuram, MD1, Sana Afreen Ansari, MD1, Saisree Reddy Adla Jala, MD1, Amirmohsen Arbabi, MD1, Rewanth Katamreddy, MD2, Adarsha Bajracharya, MD1, Moshen Kheradpezhouh, MD1
1Centinela Hospital Medical Center, Los Angeles, CA; 2NYMC - Saint Michael's Medical Center, New Jersey, NJ
Introduction: Acute appendicitis is a commonly encountered emergency, that can be complicated by perforation and subsequent sepsis. Our cases explores an atypical presentation of perforated appendicitis leading to sepsis and hyperbilirubinemia requiring specific treatment goals.
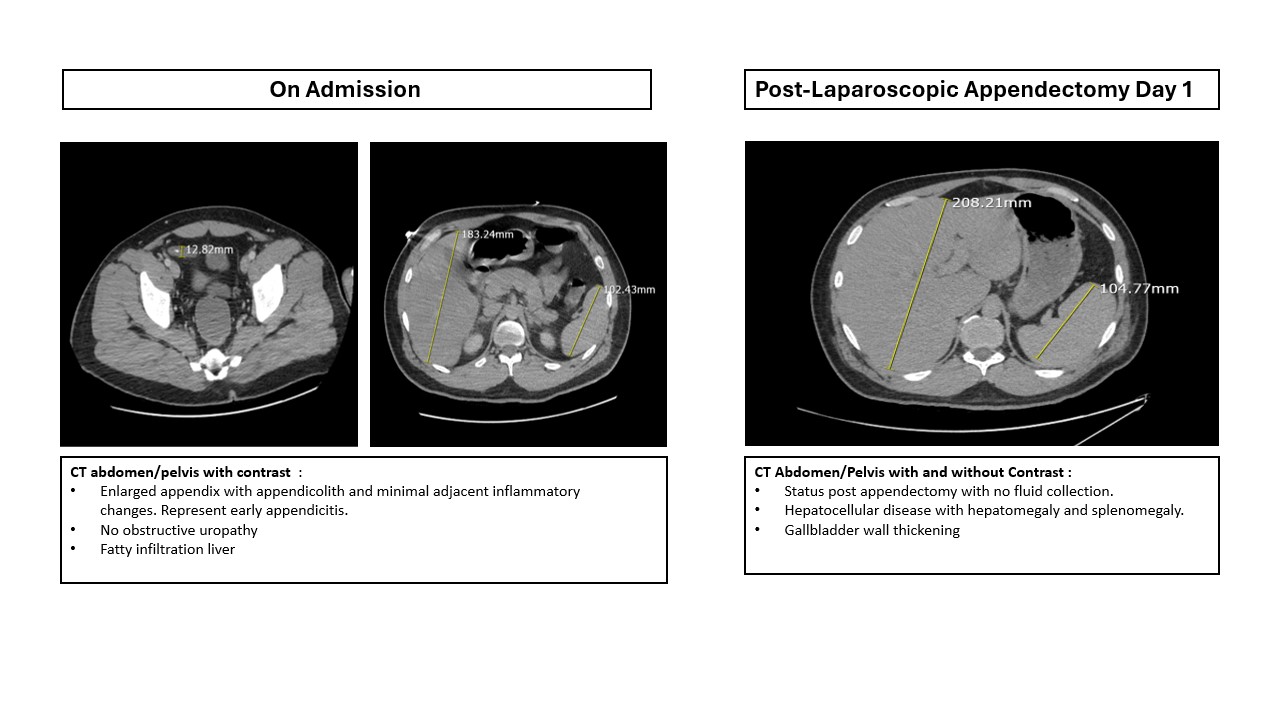
Case Description/Methods: 45-year-old Hispanic man with no pertinent past medical history was admitted with complaints of worsening abdominal pain, fever with chills, nausea, and nonbloody-nonbilious vomiting. Reportedly, the abdominal pain started a day prior to presentation, was periumbilical, rated 10/10 in intensity. While in the emergency room, he was noted to be weak, lethargic, confused, and hypotensive. Sepsis protocol was initiated, and he received IV fluid bolus along with IV ceftriaxone. Physical examination revealed diffuse abdominal tenderness and positive Murphy’s sign. Initial CT abdomen/pelvis without contrast showed an inflamed appendix measuring 12mm, consistent with acute appendicitis. The scan also revealed fatty liver changes. Surgical consultation was obtained for an emergency laparoscopic appendectomy. Operative findings and the pathology report confirmed a perforated appendix with fluid collection.
Post-operatively, he initially progressed well. Liver findings were discussed with him, and he denied any history of alcohol, tobacco, or drug use. However, on postoperative day-two, he was noted to be jaundiced with elevated total bilirubin levels of 9.4 mg/dL, up from 2.6 mg/dL on admission. Gastroenterology was consulted and MRCP was performed, which showed no bile duct obstruction or dilation.Consequently, an infectious disease (ID) consultation was obtained for positive blood culture results, which grew Escherichia coli & Bacteroides fragilis. Upon ID recommendation,IV antibiotics switched from ceftriaxone to piperacillin-tazobactam (Zosyn).Over the subsequent days, he showed improvement in appearance and a downtrend in total bilirubin levels.
He was able to tolerate a diet,remained clinically stable, and was discharged with a two-week course of IV Zosyn, followed by oral levofloxacin & metronidazole course.Outpatient follow-up arranged for further evaluation of hepatitis and monitoring of bilirubin levels.
Discussion: Drug-induced liver injury (DILI) is studied in less than 3% of patients receiving IV ceftriaxone. The literature shows that ceftriaxone could exacerbate cholestasis, with symptoms starting within a few days of initiating therapy and typically resolving once ceftriaxone is stopped.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nikitha Chellapuram, MD1, Sana Afreen Ansari, MD1, Saisree Reddy Adla Jala, MD1, Amirmohsen Arbabi, MD1, Rewanth Katamreddy, MD2, Adarsha Bajracharya, MD1, Moshen Kheradpezhouh, MD1. P4833 - Beyond Routine: Challenges in Acute Appendicitis with Gangrenous Perforation and Sepsis Complicated by Hyperbilirubinemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Centinela Hospital Medical Center, Los Angeles, CA; 2NYMC - Saint Michael's Medical Center, New Jersey, NJ
Introduction: Acute appendicitis is a commonly encountered emergency, that can be complicated by perforation and subsequent sepsis. Our cases explores an atypical presentation of perforated appendicitis leading to sepsis and hyperbilirubinemia requiring specific treatment goals.
Case Description/Methods: 45-year-old Hispanic man with no pertinent past medical history was admitted with complaints of worsening abdominal pain, fever with chills, nausea, and nonbloody-nonbilious vomiting. Reportedly, the abdominal pain started a day prior to presentation, was periumbilical, rated 10/10 in intensity. While in the emergency room, he was noted to be weak, lethargic, confused, and hypotensive. Sepsis protocol was initiated, and he received IV fluid bolus along with IV ceftriaxone. Physical examination revealed diffuse abdominal tenderness and positive Murphy’s sign. Initial CT abdomen/pelvis without contrast showed an inflamed appendix measuring 12mm, consistent with acute appendicitis. The scan also revealed fatty liver changes. Surgical consultation was obtained for an emergency laparoscopic appendectomy. Operative findings and the pathology report confirmed a perforated appendix with fluid collection.
Post-operatively, he initially progressed well. Liver findings were discussed with him, and he denied any history of alcohol, tobacco, or drug use. However, on postoperative day-two, he was noted to be jaundiced with elevated total bilirubin levels of 9.4 mg/dL, up from 2.6 mg/dL on admission. Gastroenterology was consulted and MRCP was performed, which showed no bile duct obstruction or dilation.Consequently, an infectious disease (ID) consultation was obtained for positive blood culture results, which grew Escherichia coli & Bacteroides fragilis. Upon ID recommendation,IV antibiotics switched from ceftriaxone to piperacillin-tazobactam (Zosyn).Over the subsequent days, he showed improvement in appearance and a downtrend in total bilirubin levels.
He was able to tolerate a diet,remained clinically stable, and was discharged with a two-week course of IV Zosyn, followed by oral levofloxacin & metronidazole course.Outpatient follow-up arranged for further evaluation of hepatitis and monitoring of bilirubin levels.
Discussion: Drug-induced liver injury (DILI) is studied in less than 3% of patients receiving IV ceftriaxone. The literature shows that ceftriaxone could exacerbate cholestasis, with symptoms starting within a few days of initiating therapy and typically resolving once ceftriaxone is stopped.
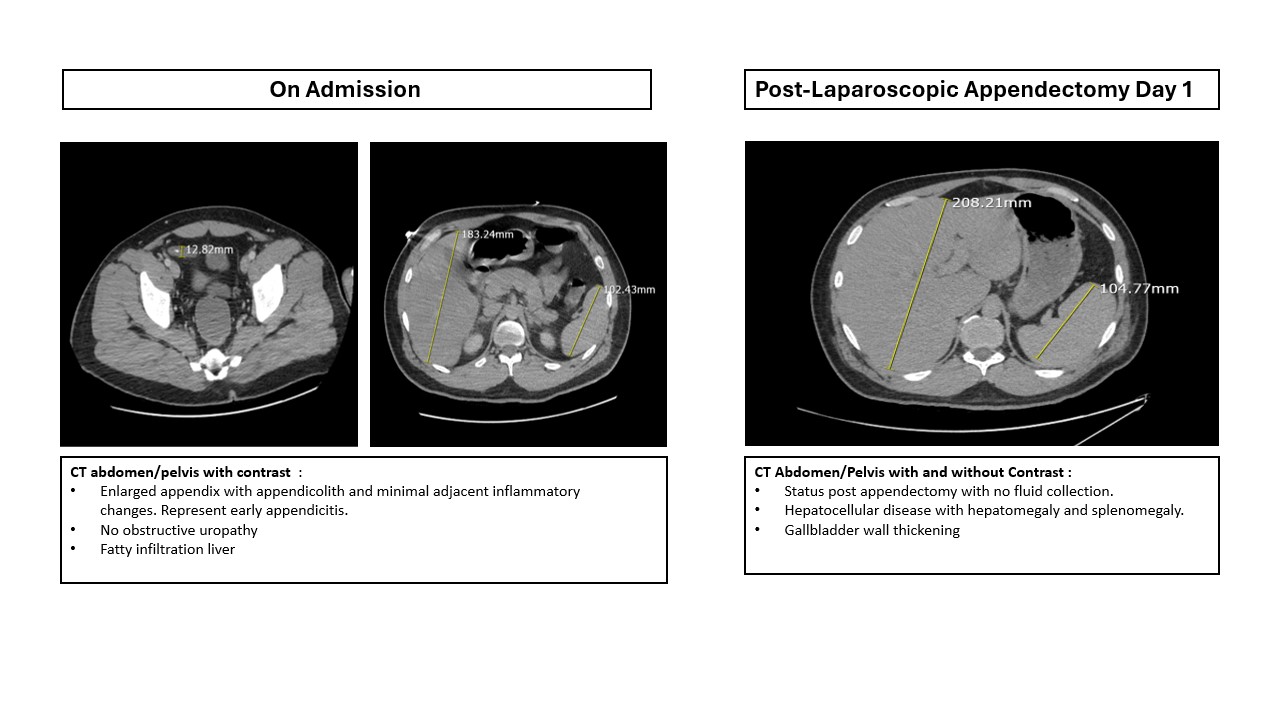
Figure: Diagnostic Imaging on right shows the evidence of acute appendicitis and fatty liver disease, while on the left shows Hepatomegaly and Splenomegaly likely secondary to Drug-Induced Liver Injury (DILI) noted after IV Ceftriaxone therapy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nikitha Chellapuram indicated no relevant financial relationships.
Sana Afreen Ansari indicated no relevant financial relationships.
Saisree Reddy Adla Jala indicated no relevant financial relationships.
Amirmohsen Arbabi indicated no relevant financial relationships.
Rewanth Katamreddy indicated no relevant financial relationships.
Adarsha Bajracharya indicated no relevant financial relationships.
Moshen Kheradpezhouh indicated no relevant financial relationships.
Nikitha Chellapuram, MD1, Sana Afreen Ansari, MD1, Saisree Reddy Adla Jala, MD1, Amirmohsen Arbabi, MD1, Rewanth Katamreddy, MD2, Adarsha Bajracharya, MD1, Moshen Kheradpezhouh, MD1. P4833 - Beyond Routine: Challenges in Acute Appendicitis with Gangrenous Perforation and Sepsis Complicated by Hyperbilirubinemia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
