Tuesday Poster Session
Category: Liver
P4844 - Perplexing “Pseudotumoral” Findings in Acute Alcohol-Associated Hepatitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- LV
Lindsay Valenti, MD
University of California Davis Health
Sacramento, CA
Presenting Author(s)
Award: Presidential Poster Award
Lindsay Valenti, MD, Vikrant Rachakonda, MD
University of California Davis Health, Sacramento, CA
Introduction: Acute alcohol-associated hepatitis (AAH) is a serious form of alcohol-associated liver disease (ALD), often complicated by coagulopathy, ascites, portal hypertension and varices, hepatic encephalopathy, and high rates of mortality in severe cases. A lesser-known complication can be found in imaging studies: a heterogenous “pseudotumoral” appearance of liver parenchyma that can mimic primary intrahepatic malignancies.
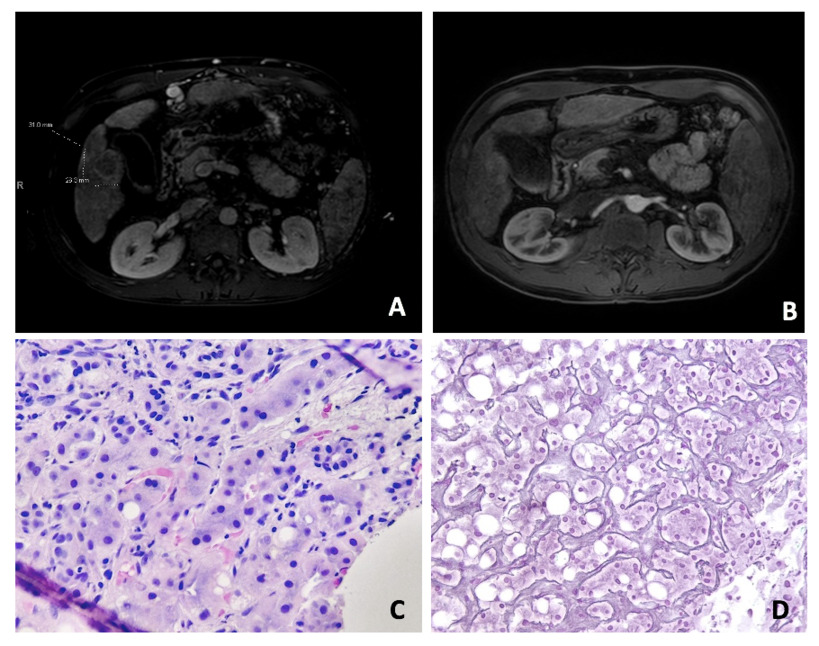
Case Description/Methods: A 40-year-old man with a history of alcohol use disorder presented with jaundice, abdominal pain, and cholestatic liver injury in the setting of sustained alcohol use. Maddrey Discriminant Function was 112, MELD 3.0 was 31, with serum bilirubin >20 mg/dl and blood phosphatidylethanol level 784 ng/ml. Contrast-enhanced abdominal CT demonstrated nodular liver, ascites, splenomegaly, and varices. The study also revealed a 2.5 cm intrahepatic mass with enhancing rim in arterial phase, concerning for either hepatocellular carcinoma or cholangiocarcinoma. Tumor markers showed normal AFP, elevated CEA (7.9 ng/ml) and elevated CA 19-9 (316 ng/ml). He then underwent a liver MRI which revealed an exophytic area of abnormal enhancement measuring 3.1cm described as a LiRADS-4 tumor (Image A). Targeted biopsy of this lesion was performed given concern for malignancy in AAH with cirrhosis. However, biopsy did not reveal evidence of neoplasia but rather parenchymal collapse, severe ductal reaction, neutrophilic satellitosis, ballooning degeneration, and Mallory bodies—findings consistent with alcoholic hepatitis and cholestatic injury (Images C-D). Repeat imaging three months later revealed that the mass-like lesion had fully resolved (Image B).
Discussion: This case highlights a rare finding of a “pseudotumoral” appearance of the liver parenchyma in acute alcohol-associated hepatitis. These mass-like lesions present a diagnostic challenge and require a multidisciplinary collaboration to guide diagnosis. Described as focal hypervascular areas, they may appear similar to the heterogeneous patterns seen in hepatocellular carcinoma. As in our case, tumor markers may also be elevated and add to the uncertainty of assessing for inflammatory changes versus a malignant process. Biopsy of these lesions, however, reveals evidence of inflammation and hallmark features consistent with AAH. Management involves alcohol cessation, supportive care, and ultimately time as these lesions may spontaneously resolve as in our patient.
Disclosures:
Lindsay Valenti, MD, Vikrant Rachakonda, MD. P4844 - Perplexing “Pseudotumoral” Findings in Acute Alcohol-Associated Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Lindsay Valenti, MD, Vikrant Rachakonda, MD
University of California Davis Health, Sacramento, CA
Introduction: Acute alcohol-associated hepatitis (AAH) is a serious form of alcohol-associated liver disease (ALD), often complicated by coagulopathy, ascites, portal hypertension and varices, hepatic encephalopathy, and high rates of mortality in severe cases. A lesser-known complication can be found in imaging studies: a heterogenous “pseudotumoral” appearance of liver parenchyma that can mimic primary intrahepatic malignancies.
Case Description/Methods: A 40-year-old man with a history of alcohol use disorder presented with jaundice, abdominal pain, and cholestatic liver injury in the setting of sustained alcohol use. Maddrey Discriminant Function was 112, MELD 3.0 was 31, with serum bilirubin >20 mg/dl and blood phosphatidylethanol level 784 ng/ml. Contrast-enhanced abdominal CT demonstrated nodular liver, ascites, splenomegaly, and varices. The study also revealed a 2.5 cm intrahepatic mass with enhancing rim in arterial phase, concerning for either hepatocellular carcinoma or cholangiocarcinoma. Tumor markers showed normal AFP, elevated CEA (7.9 ng/ml) and elevated CA 19-9 (316 ng/ml). He then underwent a liver MRI which revealed an exophytic area of abnormal enhancement measuring 3.1cm described as a LiRADS-4 tumor (Image A). Targeted biopsy of this lesion was performed given concern for malignancy in AAH with cirrhosis. However, biopsy did not reveal evidence of neoplasia but rather parenchymal collapse, severe ductal reaction, neutrophilic satellitosis, ballooning degeneration, and Mallory bodies—findings consistent with alcoholic hepatitis and cholestatic injury (Images C-D). Repeat imaging three months later revealed that the mass-like lesion had fully resolved (Image B).
Discussion: This case highlights a rare finding of a “pseudotumoral” appearance of the liver parenchyma in acute alcohol-associated hepatitis. These mass-like lesions present a diagnostic challenge and require a multidisciplinary collaboration to guide diagnosis. Described as focal hypervascular areas, they may appear similar to the heterogeneous patterns seen in hepatocellular carcinoma. As in our case, tumor markers may also be elevated and add to the uncertainty of assessing for inflammatory changes versus a malignant process. Biopsy of these lesions, however, reveals evidence of inflammation and hallmark features consistent with AAH. Management involves alcohol cessation, supportive care, and ultimately time as these lesions may spontaneously resolve as in our patient.
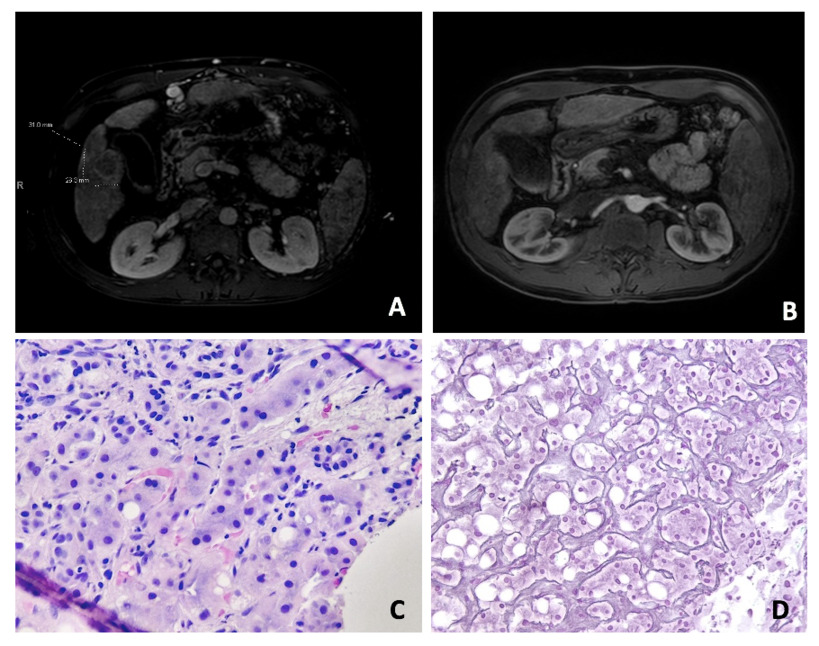
Figure: A: Initial Liver MRI (Axial View)
B: Repeat Liver MRI (Axial View)
C-D: Liver Biopsy Pathology
B: Repeat Liver MRI (Axial View)
C-D: Liver Biopsy Pathology
Disclosures:
Lindsay Valenti indicated no relevant financial relationships.
Vikrant Rachakonda indicated no relevant financial relationships.
Lindsay Valenti, MD, Vikrant Rachakonda, MD. P4844 - Perplexing “Pseudotumoral” Findings in Acute Alcohol-Associated Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


