Tuesday Poster Session
Category: Liver
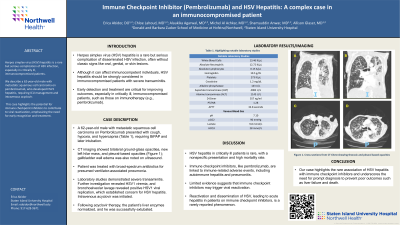
P4856 - Immune Checkpoint Inhibitor (Pembrolizumab) and HSV Hepatitis: A Complex Case in an Immunocompromised Patient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Erica Abidor, DO
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Erica Abidor, DO, Shamsuddin Anwar, MD, Allison Glaser, MD, Chloe Lahoud, MD, Alaukika Agarwal, MD, Michel Al Achkar, MD
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Herpes simplex virus (HSV) hepatitis is a rare complication of disseminated HSV infection. This condition often lacks the classic signs, such as oral, genital, or skin lesions, making diagnosis challenging. HSV hepatitis should be strongly considered in immunocompromised patients with severe transaminitis.
Case Description/Methods: A 62-year-old male with a history of metastatic squamous cell carcinoma of the oropharynx on active immunotherapy with Pembrolizumab, primary squamous cell carcinoma of the left lung (in remission), Hodgkin’s lymphoma (in remission), chronic obstructive pulmonary disease, and chronic hepatitis C presented to the hospital with a cough for five days. On admission, vital signs were notable for tachycardia to 101 bpm and rectal temperature of 95.5 °F. Laboratory studies revealed elevated pCO2, requiring BiPAP. (Table 1)
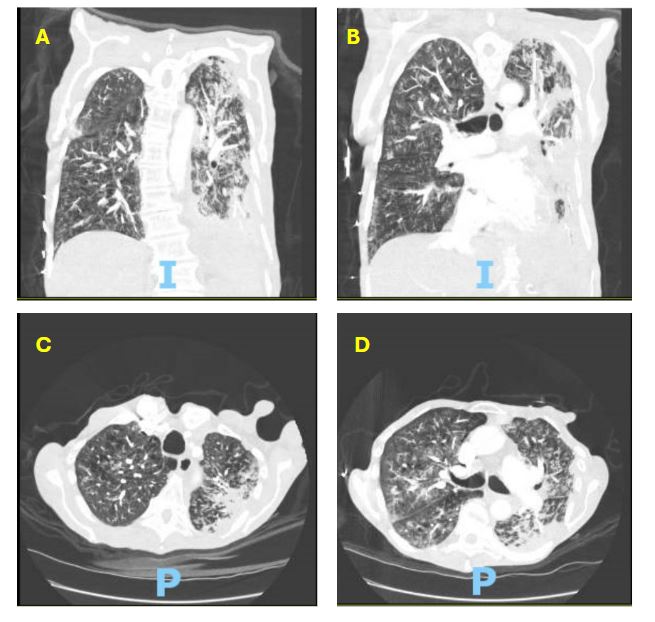
CT angiography of the chest showed multiple bilateral ground glass and pleural-based opacities in the left hemithorax (Image 1), along with a new left hilar mass/lymphadenopathy. Ultrasound of the upper right quadrant showed gallbladder wall edema.
The patient required intubation and mechanical ventilation due to increasing pCO2 on blood gases. He was managed for presumed ventilator associated pneumonia with broad spectrum antibiotics. For severe transaminitis, an extensive infectious workup revealed positive HSV1 viremia. Bronchoscopy revealed positive HSV DNA. He was promptly initiated on intravenous acyclovir. Liver biopsy was offered but declined. Eventually, the patient finished acyclovir therapy with normalization of the liver enzymes and successful extubation.
Discussion: HSV hepatitis in critically ill patients is a rare condition, with a nonspecific presentation and high mortality rate. As such, early suspicion and prompt treatment are crucial for improving patient outcomes.
Immune checkpoint inhibitors such as pembrolizumab may be associated with immune-related adverse events such as autoimmune hepatitis and pneumonitis. Limited data suggest that immune checkpoint inhibitors may be associated with the reactivation of viral syndromes, including hepatitis B. However, the association of these inhibitors with the reactivation and dissemination of HSV, leading to acute hepatitis, has been infrequently reported. Our case highlights the rare association of HSV hepatitis with immune checkpoint inhibitors and underscores the need for prompt diagnosis to prevent poor outcomes such as liver failure and death.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Erica Abidor, DO, Shamsuddin Anwar, MD, Allison Glaser, MD, Chloe Lahoud, MD, Alaukika Agarwal, MD, Michel Al Achkar, MD. P4856 - Immune Checkpoint Inhibitor (Pembrolizumab) and HSV Hepatitis: A Complex Case in an Immunocompromised Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Herpes simplex virus (HSV) hepatitis is a rare complication of disseminated HSV infection. This condition often lacks the classic signs, such as oral, genital, or skin lesions, making diagnosis challenging. HSV hepatitis should be strongly considered in immunocompromised patients with severe transaminitis.
Case Description/Methods: A 62-year-old male with a history of metastatic squamous cell carcinoma of the oropharynx on active immunotherapy with Pembrolizumab, primary squamous cell carcinoma of the left lung (in remission), Hodgkin’s lymphoma (in remission), chronic obstructive pulmonary disease, and chronic hepatitis C presented to the hospital with a cough for five days. On admission, vital signs were notable for tachycardia to 101 bpm and rectal temperature of 95.5 °F. Laboratory studies revealed elevated pCO2, requiring BiPAP. (Table 1)
CT angiography of the chest showed multiple bilateral ground glass and pleural-based opacities in the left hemithorax (Image 1), along with a new left hilar mass/lymphadenopathy. Ultrasound of the upper right quadrant showed gallbladder wall edema.
The patient required intubation and mechanical ventilation due to increasing pCO2 on blood gases. He was managed for presumed ventilator associated pneumonia with broad spectrum antibiotics. For severe transaminitis, an extensive infectious workup revealed positive HSV1 viremia. Bronchoscopy revealed positive HSV DNA. He was promptly initiated on intravenous acyclovir. Liver biopsy was offered but declined. Eventually, the patient finished acyclovir therapy with normalization of the liver enzymes and successful extubation.
Discussion: HSV hepatitis in critically ill patients is a rare condition, with a nonspecific presentation and high mortality rate. As such, early suspicion and prompt treatment are crucial for improving patient outcomes.
Immune checkpoint inhibitors such as pembrolizumab may be associated with immune-related adverse events such as autoimmune hepatitis and pneumonitis. Limited data suggest that immune checkpoint inhibitors may be associated with the reactivation of viral syndromes, including hepatitis B. However, the association of these inhibitors with the reactivation and dissemination of HSV, leading to acute hepatitis, has been infrequently reported. Our case highlights the rare association of HSV hepatitis with immune checkpoint inhibitors and underscores the need for prompt diagnosis to prevent poor outcomes such as liver failure and death.
Figure: Image 1. Cross-sections from CT Chest showing thoracic and pleural based opacities.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Erica Abidor indicated no relevant financial relationships.
Shamsuddin Anwar indicated no relevant financial relationships.
Allison Glaser indicated no relevant financial relationships.
Chloe Lahoud indicated no relevant financial relationships.
Alaukika Agarwal indicated no relevant financial relationships.
Michel Al Achkar indicated no relevant financial relationships.
Erica Abidor, DO, Shamsuddin Anwar, MD, Allison Glaser, MD, Chloe Lahoud, MD, Alaukika Agarwal, MD, Michel Al Achkar, MD. P4856 - Immune Checkpoint Inhibitor (Pembrolizumab) and HSV Hepatitis: A Complex Case in an Immunocompromised Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
