Tuesday Poster Session
Category: Liver
P4864 - Hepatosplenic Manifestations of Concomitant COVID-19 Infection and Severe Acute Babesiosis in a Healthy Adult Patient: Causality and Relationships
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Vishal Chandel, MD
Brigham and Women's Hospital, Harvard Medical School
Boston, MA
Presenting Author(s)
Vishal Chandel, MD1, Neel Chandel, MD2, Wei Yan, MD3
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Penn Medicine Princeton Medical Center, Langhorne, PA; 3Albert Einstein Medical Center, Philadelphia, PA
Introduction: Human babesiosis is a tick-borne illness by genus Babesia which resolves without complications in healthy people. The course is variable in immunocompromised patients; where ARDS, Hepatic Failure, DIC or shock can occur. Although, babesiosis is usually asymptomatic, coinfection with COVID-19 can alter the clinical course. We report a case of a healthy young female who had co-infection with COVID-19 and babesiosis altering the disease course.
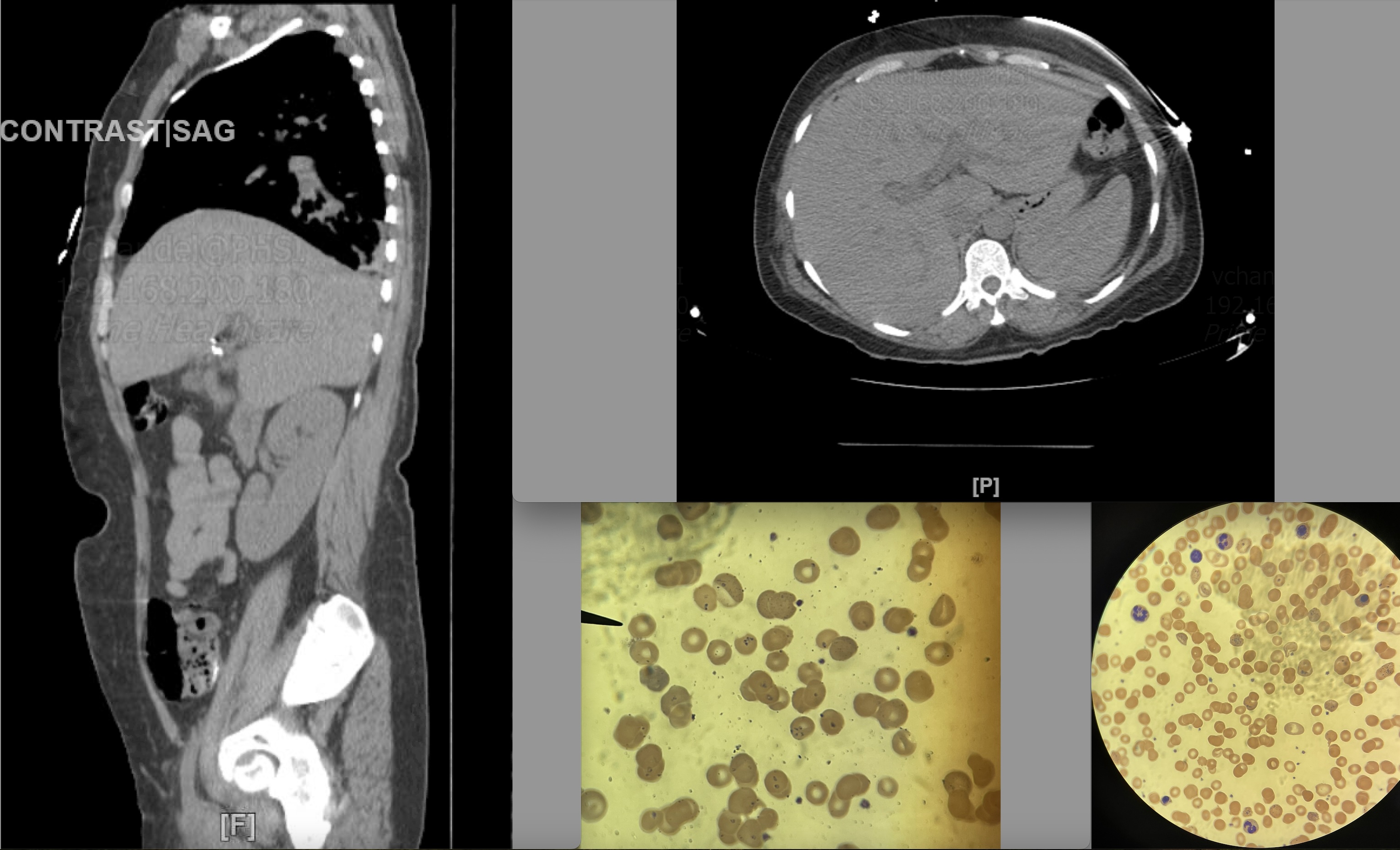
Case Description/Methods: A 46-year-old female with history of rheumatoid arthritis, COVID-19 vaccinated presented with fatigue, diarrhea, myalgias for a week. She was afebrile, hemodynamically stable, was recently diagnosed with COVID-19 and had Paxlovid for 5 days. Laboratory investigations showed anemia/thrombocytopenia and transaminitis. Imaging showed hepatosplenomegaly. Patient was given PRBC transfusion. Even after repeated transfusions, her hemoglobin dropped daily, without any active bleeding. Workup for endocarditis and viral infections including Hepatitis, HIV, EBV, and CMV was negative. Blood smear showed hemolytic anemia with intracellular ring trophozoites and 8-10% parasitemia. Initially started on intravenous artesunate for malaria, then atovaquone and azithromycin per CDC guidance, but her parasitemia stayed high. By now, her plasmodium species PCR came out negative while immunoglobulin & PCR for Babesia microti was positive. She was confirmed as acute severe babesia infection and required extended course with atovaquone, azithromycin & clindamycin. Once her hemoglobin stayed stable, transaminitis resolved and parasitemia cleared, she was discharged on 6-week course with atovaquone and azithromycin.
Discussion: Babesia-infected RBC’s have increased adhesion to capillary walls with RBC lysis causes tissue necrosis and endothelial damage. Coinfection with SARS-COV-2 virus can lead to fatal outcomes. Even though ACE2 expression (potential entry target for SARS-COV-2) is low in blood vessels and medium in liver and spleen; high parasite load in conjunction with passage of RBCs through liver and spleen can be an effective medium for increased hemolysis along with toxicity to Paxlovid lowering the immune response. Our current review of literature showed only one other report of concomitant babesiosis and COVID-19 infection. The exact pathogenic mechanisms are still unclear. Further research is needed to evaluate if there is a casualty relationship between COVID-19 infection and acute severe hemolysis and hepatosplenic manifestations in babesiosis.
Disclosures:
Vishal Chandel, MD1, Neel Chandel, MD2, Wei Yan, MD3. P4864 - Hepatosplenic Manifestations of Concomitant COVID-19 Infection and Severe Acute Babesiosis in a Healthy Adult Patient: Causality and Relationships, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 2Penn Medicine Princeton Medical Center, Langhorne, PA; 3Albert Einstein Medical Center, Philadelphia, PA
Introduction: Human babesiosis is a tick-borne illness by genus Babesia which resolves without complications in healthy people. The course is variable in immunocompromised patients; where ARDS, Hepatic Failure, DIC or shock can occur. Although, babesiosis is usually asymptomatic, coinfection with COVID-19 can alter the clinical course. We report a case of a healthy young female who had co-infection with COVID-19 and babesiosis altering the disease course.
Case Description/Methods: A 46-year-old female with history of rheumatoid arthritis, COVID-19 vaccinated presented with fatigue, diarrhea, myalgias for a week. She was afebrile, hemodynamically stable, was recently diagnosed with COVID-19 and had Paxlovid for 5 days. Laboratory investigations showed anemia/thrombocytopenia and transaminitis. Imaging showed hepatosplenomegaly. Patient was given PRBC transfusion. Even after repeated transfusions, her hemoglobin dropped daily, without any active bleeding. Workup for endocarditis and viral infections including Hepatitis, HIV, EBV, and CMV was negative. Blood smear showed hemolytic anemia with intracellular ring trophozoites and 8-10% parasitemia. Initially started on intravenous artesunate for malaria, then atovaquone and azithromycin per CDC guidance, but her parasitemia stayed high. By now, her plasmodium species PCR came out negative while immunoglobulin & PCR for Babesia microti was positive. She was confirmed as acute severe babesia infection and required extended course with atovaquone, azithromycin & clindamycin. Once her hemoglobin stayed stable, transaminitis resolved and parasitemia cleared, she was discharged on 6-week course with atovaquone and azithromycin.
Discussion: Babesia-infected RBC’s have increased adhesion to capillary walls with RBC lysis causes tissue necrosis and endothelial damage. Coinfection with SARS-COV-2 virus can lead to fatal outcomes. Even though ACE2 expression (potential entry target for SARS-COV-2) is low in blood vessels and medium in liver and spleen; high parasite load in conjunction with passage of RBCs through liver and spleen can be an effective medium for increased hemolysis along with toxicity to Paxlovid lowering the immune response. Our current review of literature showed only one other report of concomitant babesiosis and COVID-19 infection. The exact pathogenic mechanisms are still unclear. Further research is needed to evaluate if there is a casualty relationship between COVID-19 infection and acute severe hemolysis and hepatosplenic manifestations in babesiosis.
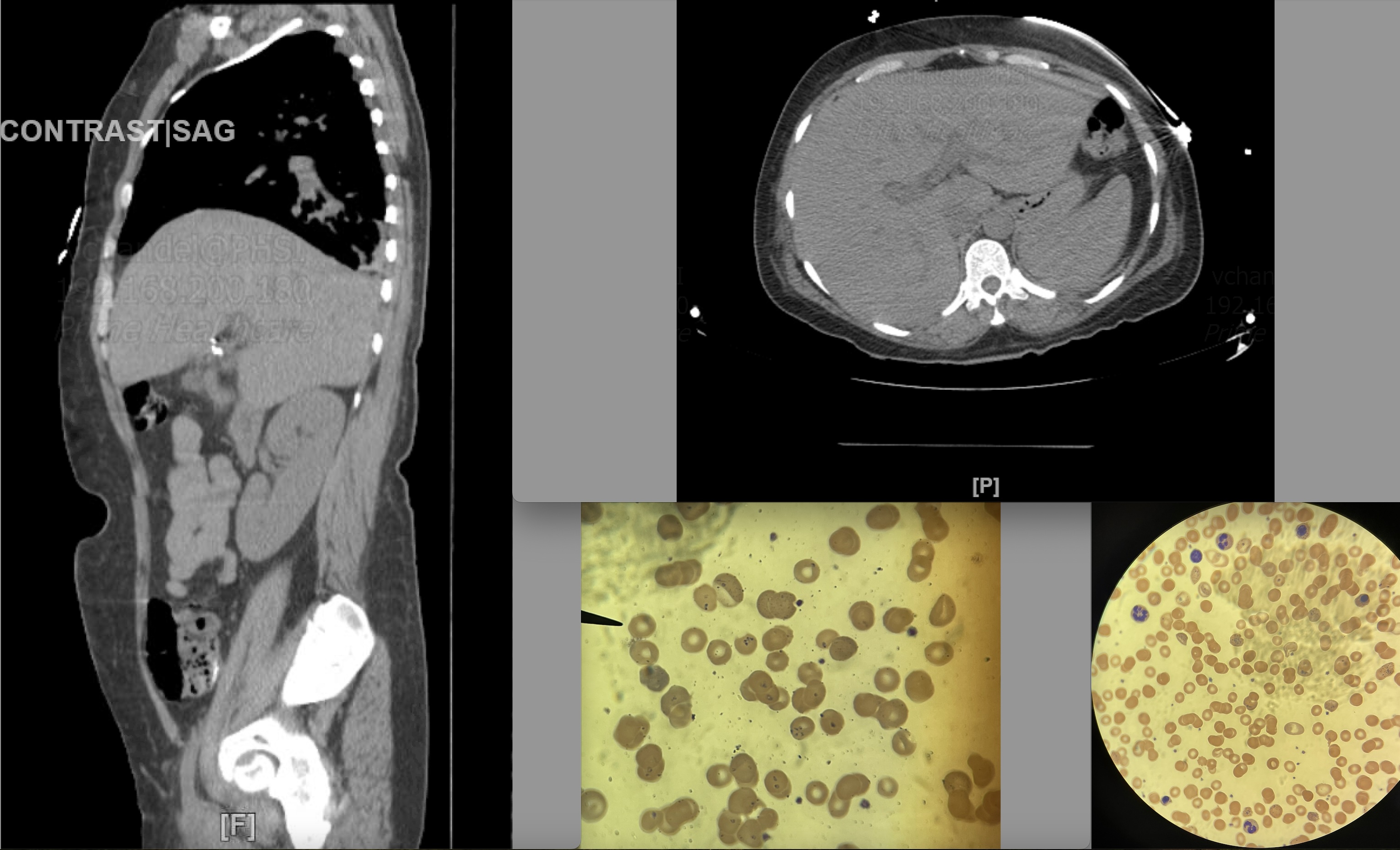
Figure: CT imaging (left, upper right) of the patient showing significant hepatosplenomegaly without any other abnormalities, lower right shows microscopic evidence of intracellular inclusions (tetrads, ring forms etc. of babesia) in red blood cells in a peripheral blood smear of patient.
Disclosures:
Vishal Chandel indicated no relevant financial relationships.
Neel Chandel indicated no relevant financial relationships.
Wei Yan indicated no relevant financial relationships.
Vishal Chandel, MD1, Neel Chandel, MD2, Wei Yan, MD3. P4864 - Hepatosplenic Manifestations of Concomitant COVID-19 Infection and Severe Acute Babesiosis in a Healthy Adult Patient: Causality and Relationships, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
