Tuesday Poster Session
Category: Obesity
P4872 - Hidden Burden of Clinical Time Required to Obtain Weight Loss Medications for Patients With MASLD
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JG
Jane Giang, PharmD
University of North Carolina Hospitals
Chapel Hill, NC
Presenting Author(s)
Jane Giang, PharmD1, Sophia Hurr, BSPH2, Alfred S. Barritt, MD, MSCR3
1University of North Carolina Hospitals, Chapel Hill, NC; 2University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 3UNC, Chapel Hill, NC
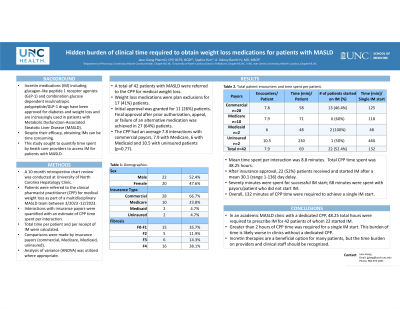
Introduction: Incretin medications (IM) including glucagon-like peptide 1 receptor agonists (GLP-1) and combination glucose dependent insulinotropic polypeptide/GLP-1 drugs have been approved for diabetes and weight loss and are increasingly used in patients with Metabolic dysfunction-Associated Steatotic Liver Disease (MASLD). Despite their efficacy, obtaining IMs can be time consuming. This study sought to quantify time spent by heath care providers to access IM for patients with MASLD.
Methods: A 10-month, single center retrospective chart review was conducted for patients referred to clinical pharmacist practitioner (CPP) for medical weight loss as part of a multidisciplinary MASLD team between 3/2023 -12/2023. Interactions with insurance payors were quantified with an estimate of CPP time spent per interaction. Total time per patient and per receipt of IM were calculated. Comparisons were made by insurance payors (commercial, Medicare, Medicaid, uninsured). Anova test was used where appropriate.
Results: A total of 42 patients with MASLD were referred to the CPP for medical weight loss. Payor types included 28 (67%) commercial plans, 10 (24%) Medicare, 2 (5%) Medicaid, and 2 (5%) uninsured. Weight loss medications were plan exclusions for 17 (41%) patients. Initial approval was granted for 11 (26%) patients. Final approval after prior authorization, appeal, or failure of an alternative medication was achieved in 27 (64%) patients. Among the 13 patients with diabetes, 4 (31%) were initially approved for IM, and 11 (85%) received final approval. The CPP had an average 7.8 interactions with commercial payors, 7.9 with Medicare, 6 with Medicaid and 10.5 with uninsured patients (p=0.77). Mean time spent per interaction was 8.8 minutes. Total CPP time spent was 48.25 hours. After insurance approval, 22 (52%) patients received and started IM after a mean 30.1 (range 1-136) day delay. Seventy minutes were spent for successful IM starts, 68 minutes were spent with payors/patients who did not start IM. Overall, 132 minutes of CPP time were required to achieve a single IM start (Table 1).
Discussion: In an academic MASLD clinic with a dedicated CPP 48.25 total hours were required to prescribe IM for 42 patients of whom 22 started IM. Greater than 2 hours of CPP time was required for a single IM start. This burden of time is likely worse in clinics without a dedicated CPP. Incretin therapies are a beneficial option for many patients, but the time burden on providers and clinical staff should be recognized.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jane Giang, PharmD1, Sophia Hurr, BSPH2, Alfred S. Barritt, MD, MSCR3. P4872 - Hidden Burden of Clinical Time Required to Obtain Weight Loss Medications for Patients With MASLD, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Carolina Hospitals, Chapel Hill, NC; 2University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC; 3UNC, Chapel Hill, NC
Introduction: Incretin medications (IM) including glucagon-like peptide 1 receptor agonists (GLP-1) and combination glucose dependent insulinotropic polypeptide/GLP-1 drugs have been approved for diabetes and weight loss and are increasingly used in patients with Metabolic dysfunction-Associated Steatotic Liver Disease (MASLD). Despite their efficacy, obtaining IMs can be time consuming. This study sought to quantify time spent by heath care providers to access IM for patients with MASLD.
Methods: A 10-month, single center retrospective chart review was conducted for patients referred to clinical pharmacist practitioner (CPP) for medical weight loss as part of a multidisciplinary MASLD team between 3/2023 -12/2023. Interactions with insurance payors were quantified with an estimate of CPP time spent per interaction. Total time per patient and per receipt of IM were calculated. Comparisons were made by insurance payors (commercial, Medicare, Medicaid, uninsured). Anova test was used where appropriate.
Results: A total of 42 patients with MASLD were referred to the CPP for medical weight loss. Payor types included 28 (67%) commercial plans, 10 (24%) Medicare, 2 (5%) Medicaid, and 2 (5%) uninsured. Weight loss medications were plan exclusions for 17 (41%) patients. Initial approval was granted for 11 (26%) patients. Final approval after prior authorization, appeal, or failure of an alternative medication was achieved in 27 (64%) patients. Among the 13 patients with diabetes, 4 (31%) were initially approved for IM, and 11 (85%) received final approval. The CPP had an average 7.8 interactions with commercial payors, 7.9 with Medicare, 6 with Medicaid and 10.5 with uninsured patients (p=0.77). Mean time spent per interaction was 8.8 minutes. Total CPP time spent was 48.25 hours. After insurance approval, 22 (52%) patients received and started IM after a mean 30.1 (range 1-136) day delay. Seventy minutes were spent for successful IM starts, 68 minutes were spent with payors/patients who did not start IM. Overall, 132 minutes of CPP time were required to achieve a single IM start (Table 1).
Discussion: In an academic MASLD clinic with a dedicated CPP 48.25 total hours were required to prescribe IM for 42 patients of whom 22 started IM. Greater than 2 hours of CPP time was required for a single IM start. This burden of time is likely worse in clinics without a dedicated CPP. Incretin therapies are a beneficial option for many patients, but the time burden on providers and clinical staff should be recognized.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Jane Giang indicated no relevant financial relationships.
Sophia Hurr indicated no relevant financial relationships.
Alfred Barritt: Boehringer Ingelheim – Consultant. Merck (Any division) – Consultant. TARGET RWE – Consultant.
Jane Giang, PharmD1, Sophia Hurr, BSPH2, Alfred S. Barritt, MD, MSCR3. P4872 - Hidden Burden of Clinical Time Required to Obtain Weight Loss Medications for Patients With MASLD, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
