Tuesday Poster Session
Category: Obesity
P4874 - Weight Loss After TORe Is Augmented by Nutritionists in an Underserved Patient Population
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Abraham Z. Cheloff, MD, MS
NYU Langone Health
New York, NY
Presenting Author(s)
Abraham Z. Cheloff, MD, MS1, Leah Kim, MD1, Manish Parikh, MD1, Rabia De Latour, MD2
1NYU Langone Health, New York, NY; 2NYU Grossman School of Medicine, New York, NY
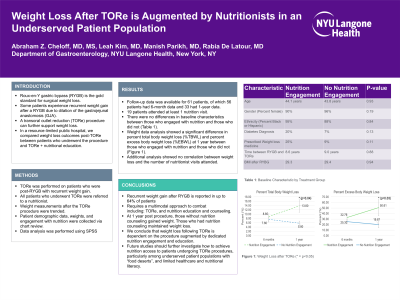
Introduction: Roux-en-Y gastric bypass (RYGB) is the gold standard for surgical weight loss. Certain patients experience recurrent weight gain or lack of sufficient weight loss after a RYGB due to dilation of the gastrojejunal anastomosis (GJA). A transoral outlet reduction (TORe) procedure can narrow the GJA, re-establish restriction, and further support weight loss. In a resource-limited public hospital, we compared weight loss outcomes post-TORe between patients who underwent the procedure alone (before the availability of nutrition services) and TORe + nutritional education, once resources were available.
Methods: TORe procedure was performed on eligible patients who were post-RYGB with recurrent weight gain. Once nutritionist resources were available, all patients who underwent TORe were referred post-procedurally. Weight measurements after the TORe procedure were followed. Patient demographic data, weights, and engagement with nutrition were collected via chart review. SPSS was utilized to perform independent t-tests comparing the patients who engaged with nutrition vs those who did not between 2018-2023.
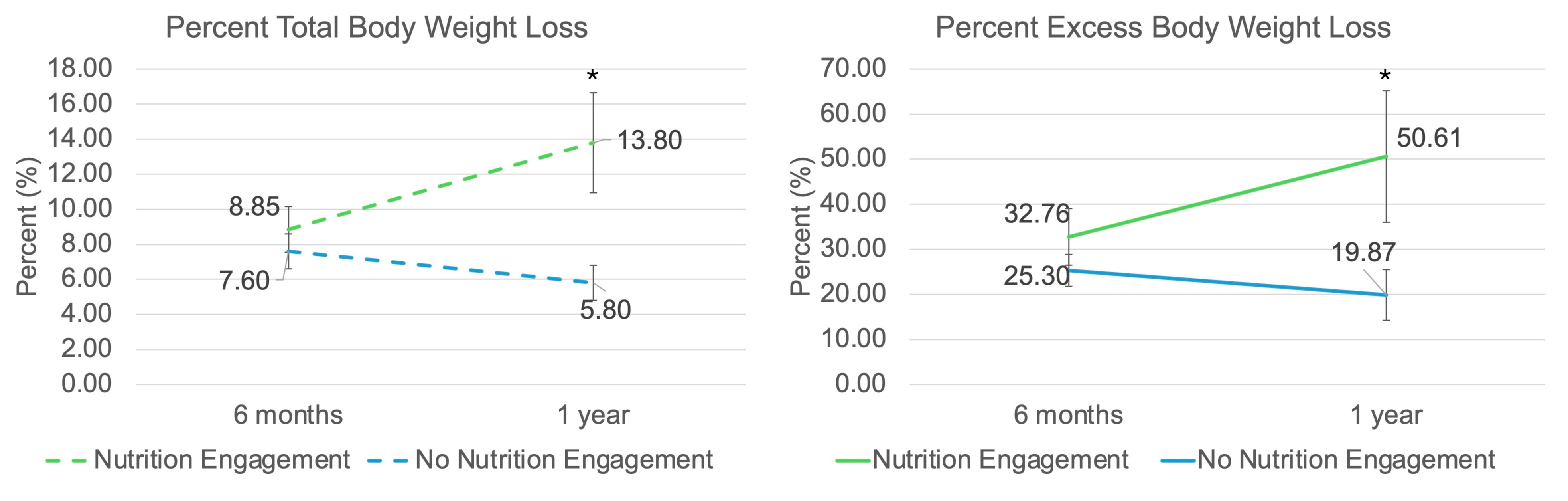
Results: Of the hundreds of patients who underwent TORe, follow-up data was available for 61 patients, of which 56 patients had 6-month data and 33 had 1-year data. Of these patients, 19 attended at least 1 nutrition visit. There were no differences in baseline characteristics between those who engaged with nutrition and those who did not (Table 1). Weight data analysis showed a significant difference in percent total body weight loss (%TBWL) and percent excess body weight loss (%EBWL) at 1 year between those who engaged with nutrition and those who did not (Figure 1). Additional analysis showed no correlation between weight loss and the number of nutritionist visits attended.
Discussion: Weight recidivism after RYGB is reported in up to 64% of patients, requiring a multimodal approach to combat including additional procedures, such as TORe, and nutrition support. Patients at 1 year without nutrition gained weight as opposed to losing weight since the procedure. We conclude that weight loss at TORe is dependent on the procedure augmented by dedicated nutrition engagement. Future studies should further investigate how to achieve nutrition access to patients undergoing TORe procedures, particularly among underserved patient populations with “food deserts”, and limited healthcare and nutritional literacy.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abraham Z. Cheloff, MD, MS1, Leah Kim, MD1, Manish Parikh, MD1, Rabia De Latour, MD2. P4874 - Weight Loss After TORe Is Augmented by Nutritionists in an Underserved Patient Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2NYU Grossman School of Medicine, New York, NY
Introduction: Roux-en-Y gastric bypass (RYGB) is the gold standard for surgical weight loss. Certain patients experience recurrent weight gain or lack of sufficient weight loss after a RYGB due to dilation of the gastrojejunal anastomosis (GJA). A transoral outlet reduction (TORe) procedure can narrow the GJA, re-establish restriction, and further support weight loss. In a resource-limited public hospital, we compared weight loss outcomes post-TORe between patients who underwent the procedure alone (before the availability of nutrition services) and TORe + nutritional education, once resources were available.
Methods: TORe procedure was performed on eligible patients who were post-RYGB with recurrent weight gain. Once nutritionist resources were available, all patients who underwent TORe were referred post-procedurally. Weight measurements after the TORe procedure were followed. Patient demographic data, weights, and engagement with nutrition were collected via chart review. SPSS was utilized to perform independent t-tests comparing the patients who engaged with nutrition vs those who did not between 2018-2023.
Results: Of the hundreds of patients who underwent TORe, follow-up data was available for 61 patients, of which 56 patients had 6-month data and 33 had 1-year data. Of these patients, 19 attended at least 1 nutrition visit. There were no differences in baseline characteristics between those who engaged with nutrition and those who did not (Table 1). Weight data analysis showed a significant difference in percent total body weight loss (%TBWL) and percent excess body weight loss (%EBWL) at 1 year between those who engaged with nutrition and those who did not (Figure 1). Additional analysis showed no correlation between weight loss and the number of nutritionist visits attended.
Discussion: Weight recidivism after RYGB is reported in up to 64% of patients, requiring a multimodal approach to combat including additional procedures, such as TORe, and nutrition support. Patients at 1 year without nutrition gained weight as opposed to losing weight since the procedure. We conclude that weight loss at TORe is dependent on the procedure augmented by dedicated nutrition engagement. Future studies should further investigate how to achieve nutrition access to patients undergoing TORe procedures, particularly among underserved patient populations with “food deserts”, and limited healthcare and nutritional literacy.
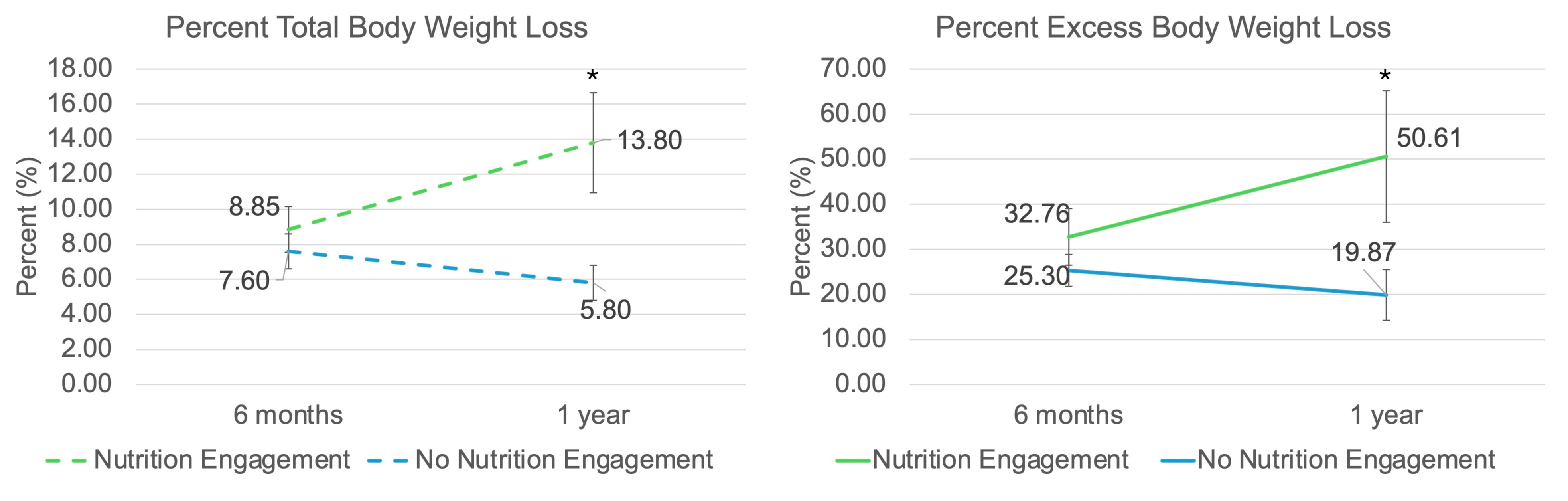
Figure: Figure 1: Weight Loss for 1 year after TORe procedure (*=p<0.05)
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abraham Cheloff indicated no relevant financial relationships.
Leah Kim indicated no relevant financial relationships.
Manish Parikh indicated no relevant financial relationships.
Rabia De Latour: Boston Sci – Speakers Bureau.
Abraham Z. Cheloff, MD, MS1, Leah Kim, MD1, Manish Parikh, MD1, Rabia De Latour, MD2. P4874 - Weight Loss After TORe Is Augmented by Nutritionists in an Underserved Patient Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

