Tuesday Poster Session
Category: Obesity
P4875 - Diagnosis of PTSD or Depression Does Not Affect Longitudinal Weight Loss Outcomes Following Monotherapy With Intragastric Balloons or Endoscopic Sleeve Gastroplasty
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Abraham Z. Cheloff, MD, MS
NYU Langone Health
New York, NY
Presenting Author(s)
Abraham Z. Cheloff, MD, MS, Leah Kim, MD, Violeta Popov, MD, PhD
NYU Langone Health, New York, NY
Introduction: Endoscopic bariatric therapies (EBTs) including intragastric balloons (IGB) and endoscopic sleeve gastroplasty (ESG) are effective means of achieving weight loss. Mental health illnesses have a complex interplay in weight change and may affect procedure efficacy in patients with EBT, though this has not yet been investigated. Therefore, we aimed to compare weight loss data in patients having undergone ESG or IGB between those with a diagnosis of depression or post-traumatic stress disorder (PTSD), and those without.
Methods: This was a retrospective study of prospectively collected data, in which patient charts at a single urban hospital between 2016-2022 who had received IGB or ESG were reviewed. It was noted whether a chart diagnosis of PTSD or Depression was present in the patient chart at any time in the study period. The primary outcome was comparing percent total body weight loss (%TBWL) and percent excess weight loss (%EWL) up to five years after the initial procedure in those with or without a mental health condition. Secondary outcomes included weight loss by procedure type and regression modeling for predictors of weight loss.
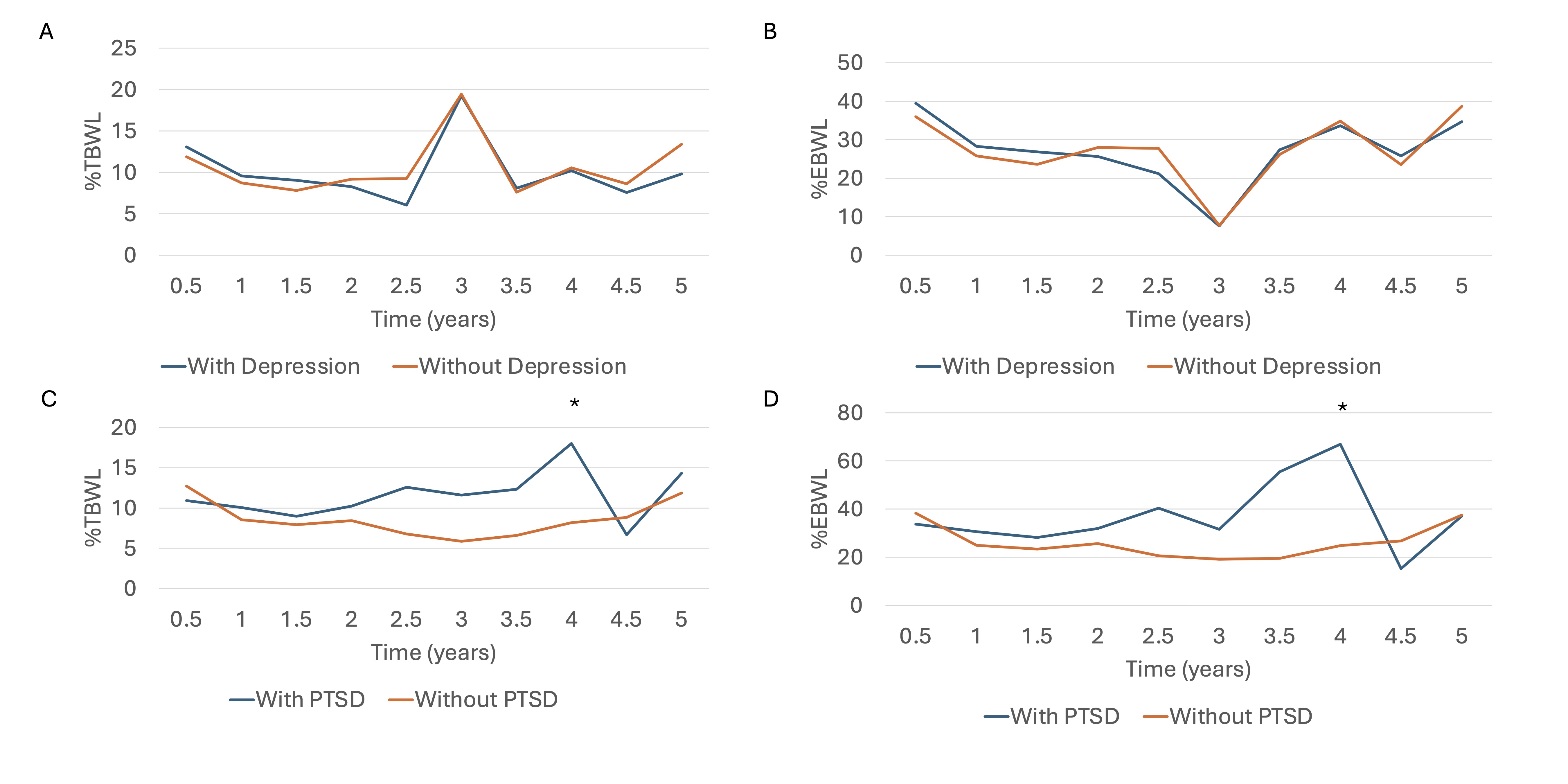
Results: Seventy-nine patients were included, of which 17 (21.5%) have a diagnosis of depression, 15 (19.0%) are diagnosed with PTSD, and 7 (8.9%) are diagnosed with both. Follow-up weight data was available for 74 at 1 year, 45 at 2 years, 28 at 3 years, 26 at 4 years, and 19 at 5 years. No significant baseline differences were seen between groups (Table 1). Weight loss over the follow-up period was not significantly different between those diagnosed with a mental health condition and those without (Figure 1). Subgroup analysis showed no significant difference at any time between IGB patients with or without depression or PTSD, and similarly in those who received ESG. Univariate regression showed significant predictors of weight loss to be baseline BMI (p=0.02) and procedure type (IGB or ESG) (p=0.01), but not a diagnosis of PTSD or depression, diabetes, or addition of weight-loss medications (Table 1).
Discussion: Weight loss in patients who received either IGB or ESG was overall unaffected by a diagnosis of PTSD or depression, but depended on baseline BMI and procedure choice. Although the treatment of mental health conditions is important for overall patient care, it does not appear to be associated with weight loss outcomes after EBT, and should not be considered a contraindication to such procedures.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abraham Z. Cheloff, MD, MS, Leah Kim, MD, Violeta Popov, MD, PhD. P4875 - Diagnosis of PTSD or Depression Does Not Affect Longitudinal Weight Loss Outcomes Following Monotherapy With Intragastric Balloons or Endoscopic Sleeve Gastroplasty, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
NYU Langone Health, New York, NY
Introduction: Endoscopic bariatric therapies (EBTs) including intragastric balloons (IGB) and endoscopic sleeve gastroplasty (ESG) are effective means of achieving weight loss. Mental health illnesses have a complex interplay in weight change and may affect procedure efficacy in patients with EBT, though this has not yet been investigated. Therefore, we aimed to compare weight loss data in patients having undergone ESG or IGB between those with a diagnosis of depression or post-traumatic stress disorder (PTSD), and those without.
Methods: This was a retrospective study of prospectively collected data, in which patient charts at a single urban hospital between 2016-2022 who had received IGB or ESG were reviewed. It was noted whether a chart diagnosis of PTSD or Depression was present in the patient chart at any time in the study period. The primary outcome was comparing percent total body weight loss (%TBWL) and percent excess weight loss (%EWL) up to five years after the initial procedure in those with or without a mental health condition. Secondary outcomes included weight loss by procedure type and regression modeling for predictors of weight loss.
Results: Seventy-nine patients were included, of which 17 (21.5%) have a diagnosis of depression, 15 (19.0%) are diagnosed with PTSD, and 7 (8.9%) are diagnosed with both. Follow-up weight data was available for 74 at 1 year, 45 at 2 years, 28 at 3 years, 26 at 4 years, and 19 at 5 years. No significant baseline differences were seen between groups (Table 1). Weight loss over the follow-up period was not significantly different between those diagnosed with a mental health condition and those without (Figure 1). Subgroup analysis showed no significant difference at any time between IGB patients with or without depression or PTSD, and similarly in those who received ESG. Univariate regression showed significant predictors of weight loss to be baseline BMI (p=0.02) and procedure type (IGB or ESG) (p=0.01), but not a diagnosis of PTSD or depression, diabetes, or addition of weight-loss medications (Table 1).
Discussion: Weight loss in patients who received either IGB or ESG was overall unaffected by a diagnosis of PTSD or depression, but depended on baseline BMI and procedure choice. Although the treatment of mental health conditions is important for overall patient care, it does not appear to be associated with weight loss outcomes after EBT, and should not be considered a contraindication to such procedures.
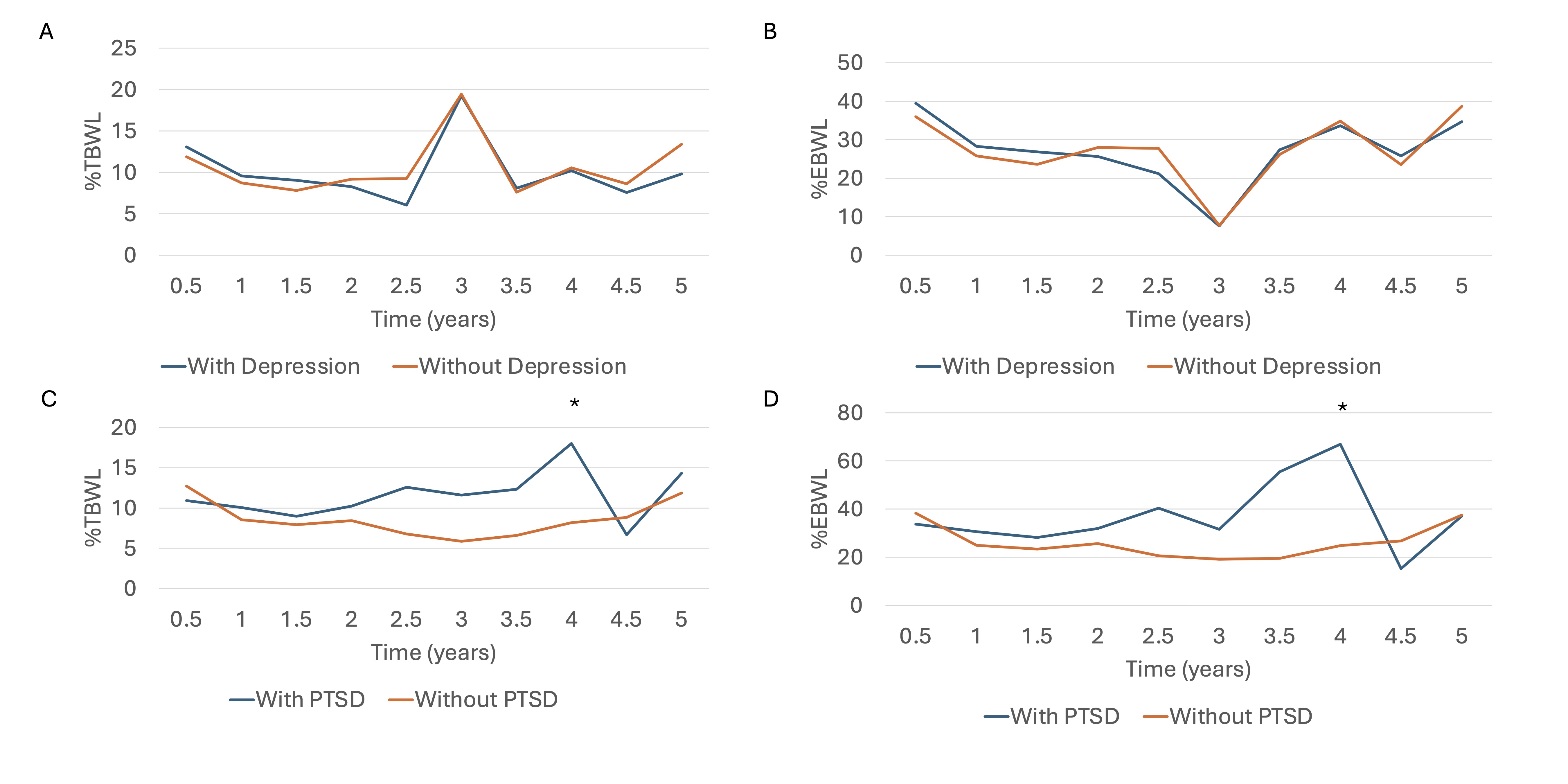
Figure: Figure 1: Weight loss outcomes over 5 years (A) %TBWL in patients with and without depression (B) %EWL in patients with and without depression (C ) %TBWL in patients with and without PTSD (D) %EWL in patients with and without PTSD
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abraham Cheloff indicated no relevant financial relationships.
Leah Kim indicated no relevant financial relationships.
Violeta Popov: MicroTech Endoscopy – Grant/Research Support.
Abraham Z. Cheloff, MD, MS, Leah Kim, MD, Violeta Popov, MD, PhD. P4875 - Diagnosis of PTSD or Depression Does Not Affect Longitudinal Weight Loss Outcomes Following Monotherapy With Intragastric Balloons or Endoscopic Sleeve Gastroplasty, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
