Tuesday Poster Session
Category: Obesity
P4878 - Visceral Adipose Tissue Density and Survival in Older Adults with Gastrointestinal Cancers
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Supriya Maheshwari, MBBS
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Supriya Maheshwari, MBBS1, Christian Harmon, MD2, Abigail Tucker, MSPH1, Apoorva Doshi, MBBS3, Ritik M. Goyal, MBBS4, Liton Francisco, BA1, Lindsey Hageman, MPH1, Smita Bhatia, MD, MPH1, El-Rayes Bassel, MD1, Grant R. Williams, MD1, Smith Giri, MD, MHS1
1University of Alabama at Birmingham, Birmingham, AL; 2Crestwood Medical Center, Huntsville, AL; 3Seth Gordhandas Sundardas Medical College and KEM Hospital, Surat, Gujarat, India; 4Rutgers New Jersey Medical School, Newark, NJ
Introduction: Lower skeletal muscle density is known to be associated with worse survival in patients with gastrointestinal (GI) cancers, but there is paucity of literature regarding the prognostic value of adipose tissue density in this population. Denser adipose tissue contains smaller adipocytes, and more fibrous matrix, which alters the metabolic activity and inflammatory state of the tissue, in turn affecting the tumor characteristics and treatment response. We aimed to study the association of visceral adipose tissue (VAT) density and overall survival (OS) in older adults with GI cancer.
Methods: We included older adults (≥60y) with newly diagnosed GI cancers enrolled in an ongoing prospective study who underwent geriatric assessment (GA) within 90 days of diagnosis with available abdominal computed tomography (CT) images within 90 days of GA. Using validated segmentation methods, we measured skeletal muscle (SM), subcutaneous adipose tissue (SAT) and VAT areas [in cm2], VAT density, and skeletal muscle density (SMD) [in Hounsfield units (HU)], at the third lumbar vertebrae (L3) level. The primary end point was OS. We used uni- and multi-variable Cox proportional hazards regression models adjusted for age, sex, cancer type, cancer stage, frailty, SM, SAT and VAT areas, and SMD to study the association between VAT density and OS in GI cancer patients.
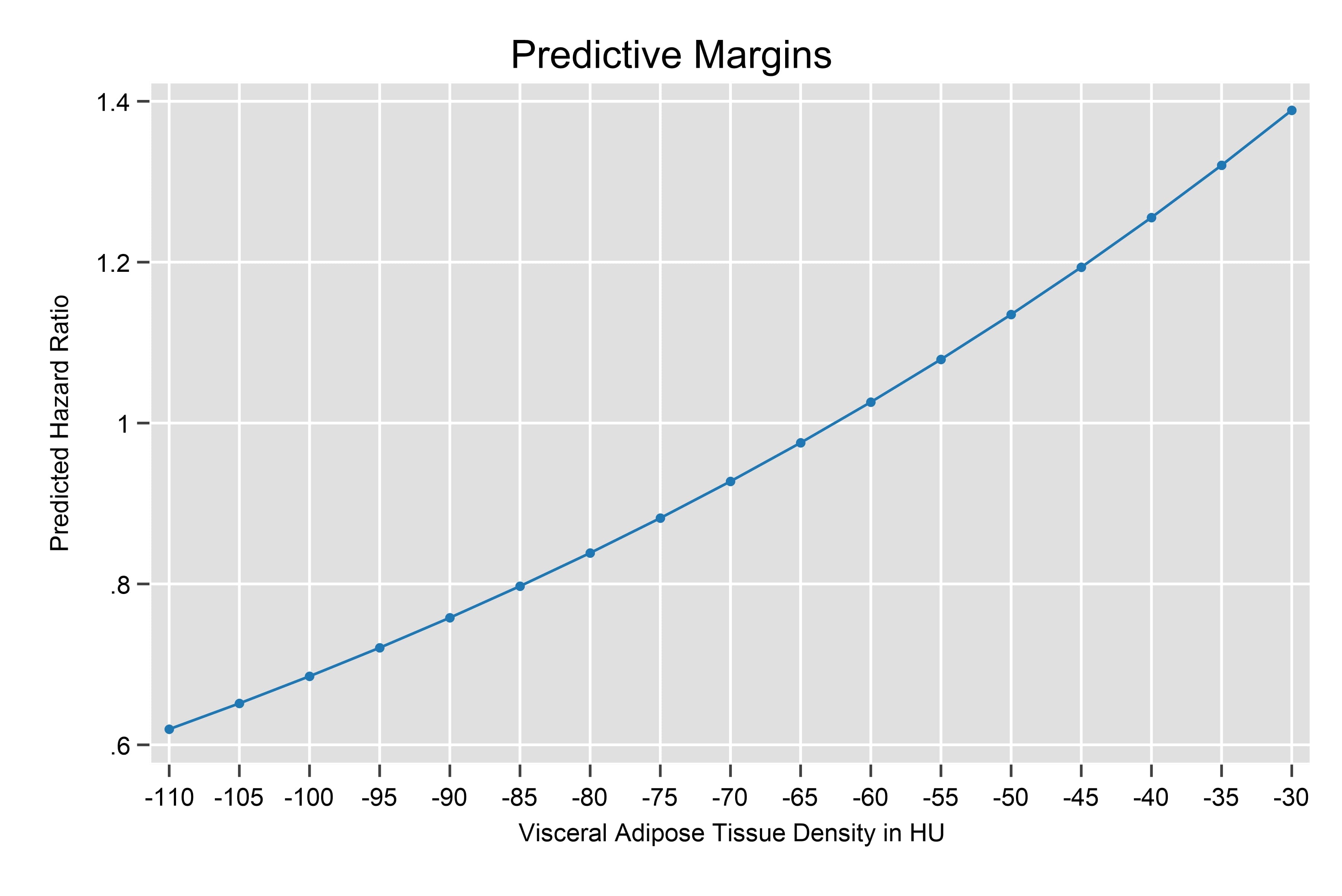
Results: Our study included 639 older adults with GI cancers; median age at study participation: 70y (Interquartile range, IQR 63-77); 56% male, 73% non-Hispanic white; most common primary diagnoses: colorectal (35%) and pancreatic cancer (26%). Median VAT density (in HU) was -84 (IQR, -92 to -75). Median follow-up period was 40.3 months, and 3y OS was 56.3% (95% CI 52.1-60.3%). In multivariable Cox model, higher VAT density was associated with inferior OS (Hazard ratio 1.18; 95% CI 1.02-1.36; p = 0.03, per 1 standard deviation increase), when adjusted for afore mentioned confounders [Figure 1], [Table 1].
Discussion: We found that higher VAT density is independently associated with worse OS in older adults with GI cancers. Further studies are required to assess the prognostic value of CT derived adipose tissue density in patients with GI cancers.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Supriya Maheshwari, MBBS1, Christian Harmon, MD2, Abigail Tucker, MSPH1, Apoorva Doshi, MBBS3, Ritik M. Goyal, MBBS4, Liton Francisco, BA1, Lindsey Hageman, MPH1, Smita Bhatia, MD, MPH1, El-Rayes Bassel, MD1, Grant R. Williams, MD1, Smith Giri, MD, MHS1. P4878 - Visceral Adipose Tissue Density and Survival in Older Adults with Gastrointestinal Cancers, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham, Birmingham, AL; 2Crestwood Medical Center, Huntsville, AL; 3Seth Gordhandas Sundardas Medical College and KEM Hospital, Surat, Gujarat, India; 4Rutgers New Jersey Medical School, Newark, NJ
Introduction: Lower skeletal muscle density is known to be associated with worse survival in patients with gastrointestinal (GI) cancers, but there is paucity of literature regarding the prognostic value of adipose tissue density in this population. Denser adipose tissue contains smaller adipocytes, and more fibrous matrix, which alters the metabolic activity and inflammatory state of the tissue, in turn affecting the tumor characteristics and treatment response. We aimed to study the association of visceral adipose tissue (VAT) density and overall survival (OS) in older adults with GI cancer.
Methods: We included older adults (≥60y) with newly diagnosed GI cancers enrolled in an ongoing prospective study who underwent geriatric assessment (GA) within 90 days of diagnosis with available abdominal computed tomography (CT) images within 90 days of GA. Using validated segmentation methods, we measured skeletal muscle (SM), subcutaneous adipose tissue (SAT) and VAT areas [in cm2], VAT density, and skeletal muscle density (SMD) [in Hounsfield units (HU)], at the third lumbar vertebrae (L3) level. The primary end point was OS. We used uni- and multi-variable Cox proportional hazards regression models adjusted for age, sex, cancer type, cancer stage, frailty, SM, SAT and VAT areas, and SMD to study the association between VAT density and OS in GI cancer patients.
Results: Our study included 639 older adults with GI cancers; median age at study participation: 70y (Interquartile range, IQR 63-77); 56% male, 73% non-Hispanic white; most common primary diagnoses: colorectal (35%) and pancreatic cancer (26%). Median VAT density (in HU) was -84 (IQR, -92 to -75). Median follow-up period was 40.3 months, and 3y OS was 56.3% (95% CI 52.1-60.3%). In multivariable Cox model, higher VAT density was associated with inferior OS (Hazard ratio 1.18; 95% CI 1.02-1.36; p = 0.03, per 1 standard deviation increase), when adjusted for afore mentioned confounders [Figure 1], [Table 1].
Discussion: We found that higher VAT density is independently associated with worse OS in older adults with GI cancers. Further studies are required to assess the prognostic value of CT derived adipose tissue density in patients with GI cancers.
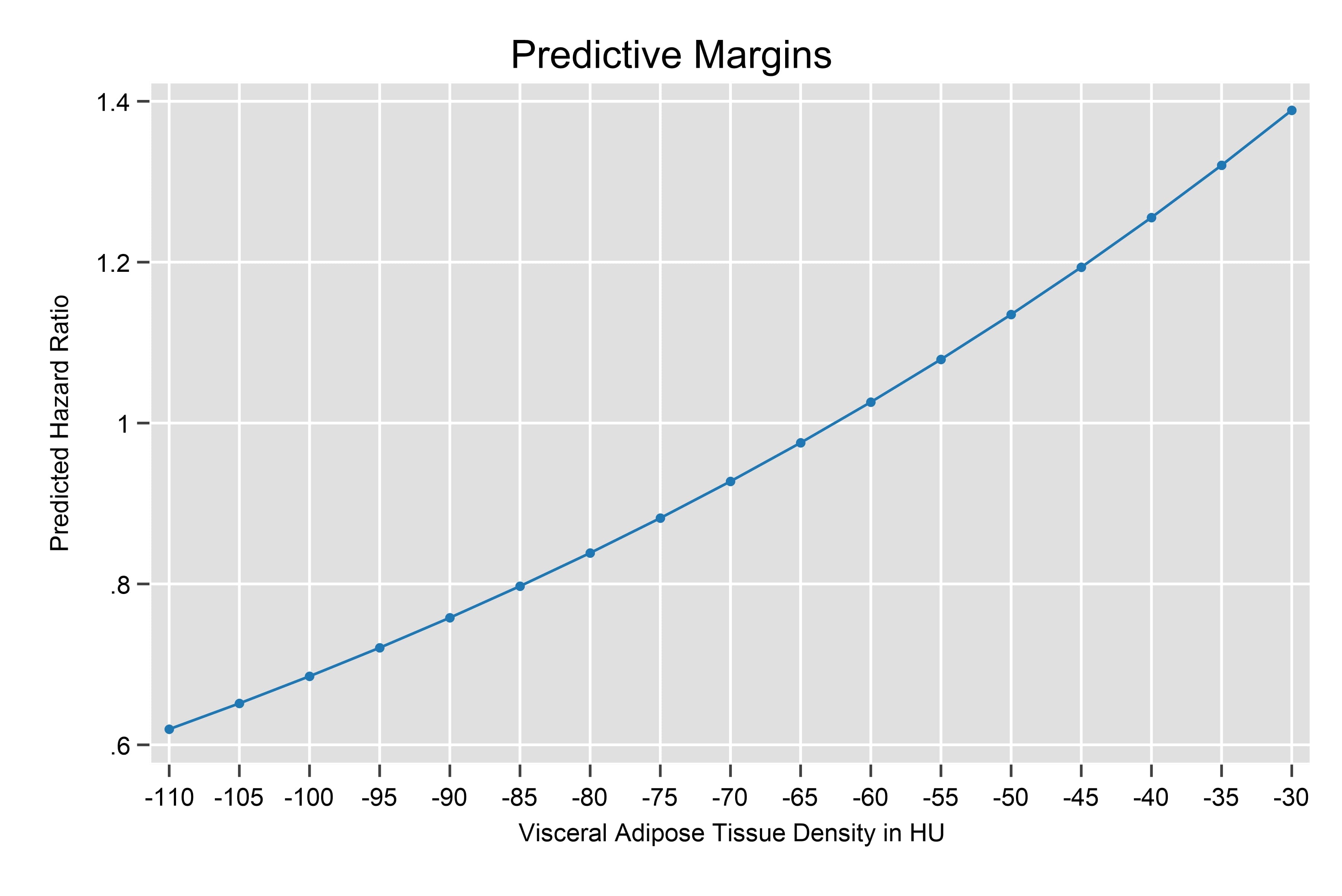
Figure: Image 1: Visceral adipose tissue density and predicted hazards ratio in gastrointestinal cancer patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Supriya Maheshwari indicated no relevant financial relationships.
Christian Harmon indicated no relevant financial relationships.
Abigail Tucker indicated no relevant financial relationships.
Apoorva Doshi indicated no relevant financial relationships.
Ritik Goyal indicated no relevant financial relationships.
Liton Francisco indicated no relevant financial relationships.
Lindsey Hageman indicated no relevant financial relationships.
Smita Bhatia indicated no relevant financial relationships.
El-Rayes Bassel indicated no relevant financial relationships.
Grant R. Williams: Bayer – Honararia. Takeda – Honararia.
Smith Giri: Carevive – Honararia. jansenn – Grant/Research Support. Onclive – Honararia. Pack Health – Grant/Research Support. Sanofi – Grant/Research Support.
Supriya Maheshwari, MBBS1, Christian Harmon, MD2, Abigail Tucker, MSPH1, Apoorva Doshi, MBBS3, Ritik M. Goyal, MBBS4, Liton Francisco, BA1, Lindsey Hageman, MPH1, Smita Bhatia, MD, MPH1, El-Rayes Bassel, MD1, Grant R. Williams, MD1, Smith Giri, MD, MHS1. P4878 - Visceral Adipose Tissue Density and Survival in Older Adults with Gastrointestinal Cancers, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
