Tuesday Poster Session
Category: Obesity
P4879 - Partnership With An Independent Telehealth Obesity Medicine Program After Endoscopic Bariatric Procedures Improves Weight Loss Outcomes At 12 Months
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- PK
Philip Kozan, MD
David Geffen School of Medicine at UCLA
Los Angeles, CA
Presenting Author(s)
Philip Kozan, MD1, Meghna Yalamanchi, MD2, Sergio A. De La Torre, MD1, Danny Issa, MD1, Alireza Sedarat, MD1, Florencia Halperin, MD, MMSc3, Adarsh Thaker, MD1, Lauren Lemieux, MD3
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2Olive View-UCLA Medical Center, Los Angeles, CA; 3Form Health, Boston, MA
Introduction: A challenge for a successful Bariatric Endoscopy program is establishing multi-disciplinary obesity medicine and nutrition support. New programs may lack access to these resources or be limited by institution/practice financial support. To overcome these barriers in our program, we partnered with an independent telemedicine obesity treatment practice to assist in the management of patients undergoing endoscopic bariatric therapies (EBT).
Methods: A prospective observational study was performed on patients that had an EBT at an academic tertiary referral center between January 2022 to July 2023. A group of patients was referred to an external program (EP), an unaffiliated, multi-disciplinary, evidence-based obesity treatment program delivered via a proprietary smartphone application. EP patients were scheduled for regular telemedicine visits with certified obesity medicine physicians monthly and licensed registered dietitians twice monthly. Internal program (IP) patients were managed by the endoscopists or referred to clinical nutrition providers internally. Weight loss outcomes were compared between EP and IP patients. Statistical analysis was done with Student’s t-test and Chi-Squared test.
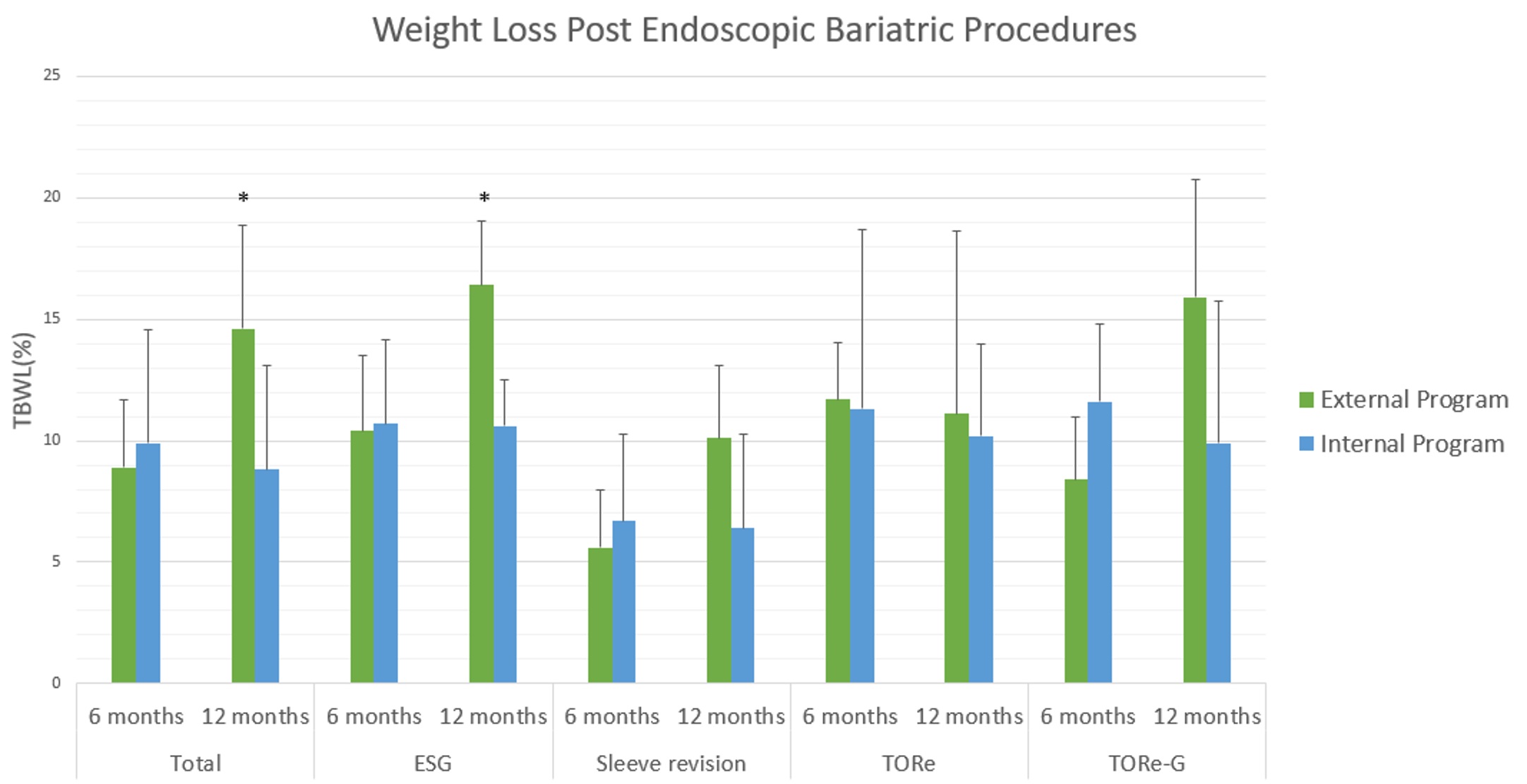
Results: A total of 225 patients underwent EBTs, of which 43 patients established with the EP. EBT procedures included endoscopic sleeve gastroplasty (ESG), surgical sleeve revision, and transoral outlet reduction (TORe) with gastroplasty (TORe-G). No significant differences in demographics or comorbidities were noted between the EP and IP patients, including pre-EBT weights (251.5±55.3 vs. 241.3±63.2 lbs., P=0.27), further described in table 1. Total body weight loss was significantly greater at 12 months in patients established with the EP (14.6±8.4 %) vs. those established in the IP (8.8±8.6%), P=0.01 (Figure 1). Subgroup analysis showed that weight loss at 12 months was driven primarily by the patients undergoing ESGs (EP 16.4±5.3 vs. IP 10.6±3.9%, P=0.01).
Discussion: Partnership with an unaffiliated external medical weight loss program was associated with significantly greater weight loss after EBTs, possibly due to higher-intensity management, improved access to care thus improving compliance, or greater use of synergistic weight loss medications. Our strategy of referring patients to a telemedicine weight loss program can serve as a useful care model for new or growing endobariatric programs who may be struggling to establish obesity medicine resources.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Philip Kozan, MD1, Meghna Yalamanchi, MD2, Sergio A. De La Torre, MD1, Danny Issa, MD1, Alireza Sedarat, MD1, Florencia Halperin, MD, MMSc3, Adarsh Thaker, MD1, Lauren Lemieux, MD3. P4879 - Partnership With An Independent Telehealth Obesity Medicine Program After Endoscopic Bariatric Procedures Improves Weight Loss Outcomes At 12 Months, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1David Geffen School of Medicine at UCLA, Los Angeles, CA; 2Olive View-UCLA Medical Center, Los Angeles, CA; 3Form Health, Boston, MA
Introduction: A challenge for a successful Bariatric Endoscopy program is establishing multi-disciplinary obesity medicine and nutrition support. New programs may lack access to these resources or be limited by institution/practice financial support. To overcome these barriers in our program, we partnered with an independent telemedicine obesity treatment practice to assist in the management of patients undergoing endoscopic bariatric therapies (EBT).
Methods: A prospective observational study was performed on patients that had an EBT at an academic tertiary referral center between January 2022 to July 2023. A group of patients was referred to an external program (EP), an unaffiliated, multi-disciplinary, evidence-based obesity treatment program delivered via a proprietary smartphone application. EP patients were scheduled for regular telemedicine visits with certified obesity medicine physicians monthly and licensed registered dietitians twice monthly. Internal program (IP) patients were managed by the endoscopists or referred to clinical nutrition providers internally. Weight loss outcomes were compared between EP and IP patients. Statistical analysis was done with Student’s t-test and Chi-Squared test.
Results: A total of 225 patients underwent EBTs, of which 43 patients established with the EP. EBT procedures included endoscopic sleeve gastroplasty (ESG), surgical sleeve revision, and transoral outlet reduction (TORe) with gastroplasty (TORe-G). No significant differences in demographics or comorbidities were noted between the EP and IP patients, including pre-EBT weights (251.5±55.3 vs. 241.3±63.2 lbs., P=0.27), further described in table 1. Total body weight loss was significantly greater at 12 months in patients established with the EP (14.6±8.4 %) vs. those established in the IP (8.8±8.6%), P=0.01 (Figure 1). Subgroup analysis showed that weight loss at 12 months was driven primarily by the patients undergoing ESGs (EP 16.4±5.3 vs. IP 10.6±3.9%, P=0.01).
Discussion: Partnership with an unaffiliated external medical weight loss program was associated with significantly greater weight loss after EBTs, possibly due to higher-intensity management, improved access to care thus improving compliance, or greater use of synergistic weight loss medications. Our strategy of referring patients to a telemedicine weight loss program can serve as a useful care model for new or growing endobariatric programs who may be struggling to establish obesity medicine resources.
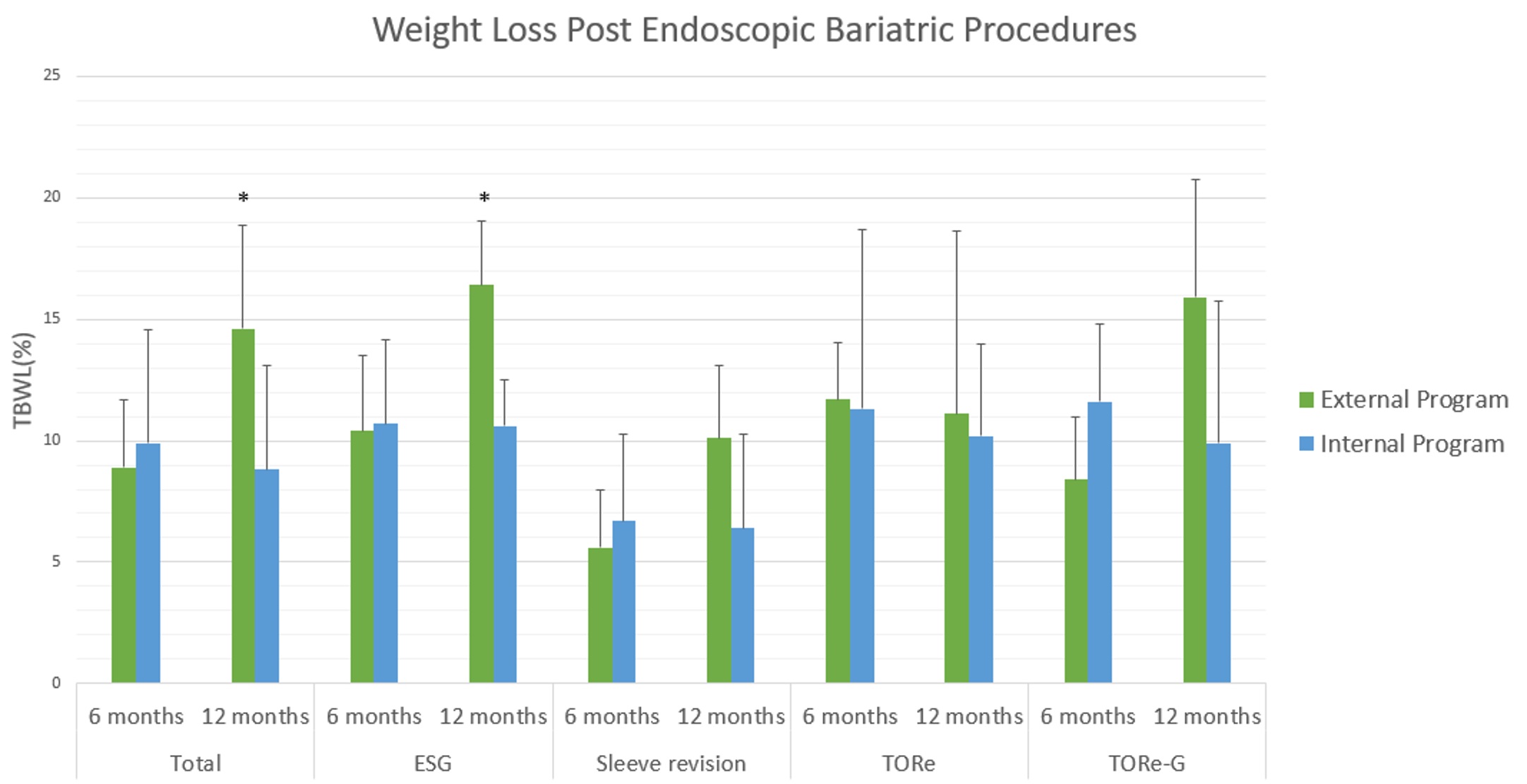
Figure: Figure 1. Weight loss trends post endoscopic weight loss procedure at 6- and 12-month intervals. ESG: Endoscopic sleeve gastroplasty; TORe: Transoral outlet reduction; TORe-G: TORe with gastroplasty. *p < 0.05
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Philip Kozan indicated no relevant financial relationships.
Meghna Yalamanchi indicated no relevant financial relationships.
Sergio De La Torre indicated no relevant financial relationships.
Danny Issa: Boston Scientific – Consultant, Speakers Bureau. Eli Lilly – Speakers Bureau.
Alireza Sedarat indicated no relevant financial relationships.
Florencia Halperin: Form Health – Employee, Stock Options.
Adarsh Thaker: Boston Scientific Corporation – Consultant, Speakers Bureau. Cook – Speakers Bureau. Fractyl Health – Grant/Research Support. Neptune Medical – Consultant. Steris – Consultant.
Lauren Lemieux indicated no relevant financial relationships.
Philip Kozan, MD1, Meghna Yalamanchi, MD2, Sergio A. De La Torre, MD1, Danny Issa, MD1, Alireza Sedarat, MD1, Florencia Halperin, MD, MMSc3, Adarsh Thaker, MD1, Lauren Lemieux, MD3. P4879 - Partnership With An Independent Telehealth Obesity Medicine Program After Endoscopic Bariatric Procedures Improves Weight Loss Outcomes At 12 Months, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
