Tuesday Poster Session
Category: Obesity
P4884 - Weight Loss Outcomes in High BMI Patients After Endoscopic Gastric Remodeling: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Noppachai Siranart, MD
Brigham and Women's Hospital
Boston, MA
Presenting Author(s)
Noppachai Siranart, MD1, Christopher C.. Thompson, MD, MSc2, Pichamol Jirapinyo, MD, MPH3
1Brigham and Women's Hospital, Boston, MA; 2Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 3Brigham and Women's Hospital, Boston, MA
Introduction: Patients with morbid obesity are at risk of potential morbidity and mortality following conventional bariatric surgery. Endoscopic gastric remodeling (EGR) has emerged as an alternative weight reduction strategy in individuals with obesity. This meta-analysis evaluated the weight loss outcomes after EGR across different obesity classifications.
Methods: A literature review was searched from inception until August 2023 to identify relevant studies. The primary outcome is comparing weight loss following EGR among individuals with varying obesity classifications at 12-months. Pooled effect estimates were computed using a random-effects model.
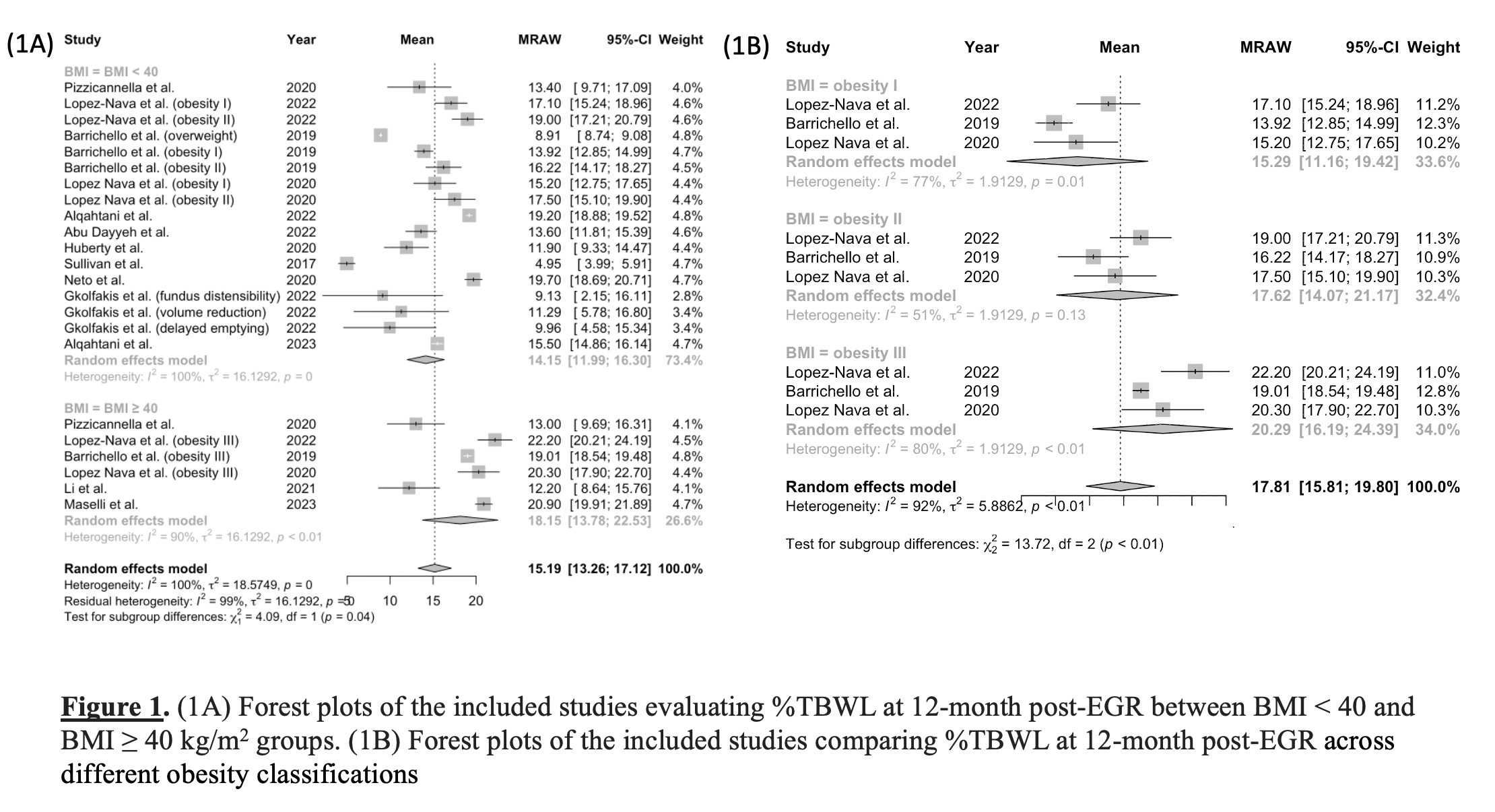
Results: A total of 14 studies were included in this meta-analysis, comprising 3 randomized trials and 11 observational studies, encompassing a total of 5,565 patients (Table 1). At 6-months post-EGR, those with body mass index (BMI) < 40 kg/m2 showed a mean total body weight loss (%TBWL) of 13.74% (95% confidence interval [CI]: 12.23–15.15%; I2 = 95%), while those with BMI ≥ 40 kg/m2 had a slightly higher reduction at 15.64% (95%CI: 11.34–19.93; I2 = 94%), with no statistically significant difference. At 12 months, patients classified as obesity class III displayed the most significant weight reduction, with a reported percentage of 20.29% (95%CI: 16.19–24.39%; I2 = 80%). In contrast, those in obesity class II exhibited a slightly lower weight reduction of 17.62% (95%CI: 14.07–21.17%; I2 = 51%), and patients in obesity class I demonstrated a reduction at 15.29% (95%CI: 11.16–19.42%; I2 = 77%) (p-value < 0.01) (Figure 1).
Discussion: EGR demonstrated satisfactory weight loss results, with obesity class III achieving significantly greater weight reduction when compared to class I and II at 12 months. These results suggest that EGR can serve as a viable treatment alternative for patients with class III obesity.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Noppachai Siranart, MD1, Christopher C.. Thompson, MD, MSc2, Pichamol Jirapinyo, MD, MPH3. P4884 - Weight Loss Outcomes in High BMI Patients After Endoscopic Gastric Remodeling: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brigham and Women's Hospital, Boston, MA; 2Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 3Brigham and Women's Hospital, Boston, MA
Introduction: Patients with morbid obesity are at risk of potential morbidity and mortality following conventional bariatric surgery. Endoscopic gastric remodeling (EGR) has emerged as an alternative weight reduction strategy in individuals with obesity. This meta-analysis evaluated the weight loss outcomes after EGR across different obesity classifications.
Methods: A literature review was searched from inception until August 2023 to identify relevant studies. The primary outcome is comparing weight loss following EGR among individuals with varying obesity classifications at 12-months. Pooled effect estimates were computed using a random-effects model.
Results: A total of 14 studies were included in this meta-analysis, comprising 3 randomized trials and 11 observational studies, encompassing a total of 5,565 patients (Table 1). At 6-months post-EGR, those with body mass index (BMI) < 40 kg/m2 showed a mean total body weight loss (%TBWL) of 13.74% (95% confidence interval [CI]: 12.23–15.15%; I2 = 95%), while those with BMI ≥ 40 kg/m2 had a slightly higher reduction at 15.64% (95%CI: 11.34–19.93; I2 = 94%), with no statistically significant difference. At 12 months, patients classified as obesity class III displayed the most significant weight reduction, with a reported percentage of 20.29% (95%CI: 16.19–24.39%; I2 = 80%). In contrast, those in obesity class II exhibited a slightly lower weight reduction of 17.62% (95%CI: 14.07–21.17%; I2 = 51%), and patients in obesity class I demonstrated a reduction at 15.29% (95%CI: 11.16–19.42%; I2 = 77%) (p-value < 0.01) (Figure 1).
Discussion: EGR demonstrated satisfactory weight loss results, with obesity class III achieving significantly greater weight reduction when compared to class I and II at 12 months. These results suggest that EGR can serve as a viable treatment alternative for patients with class III obesity.
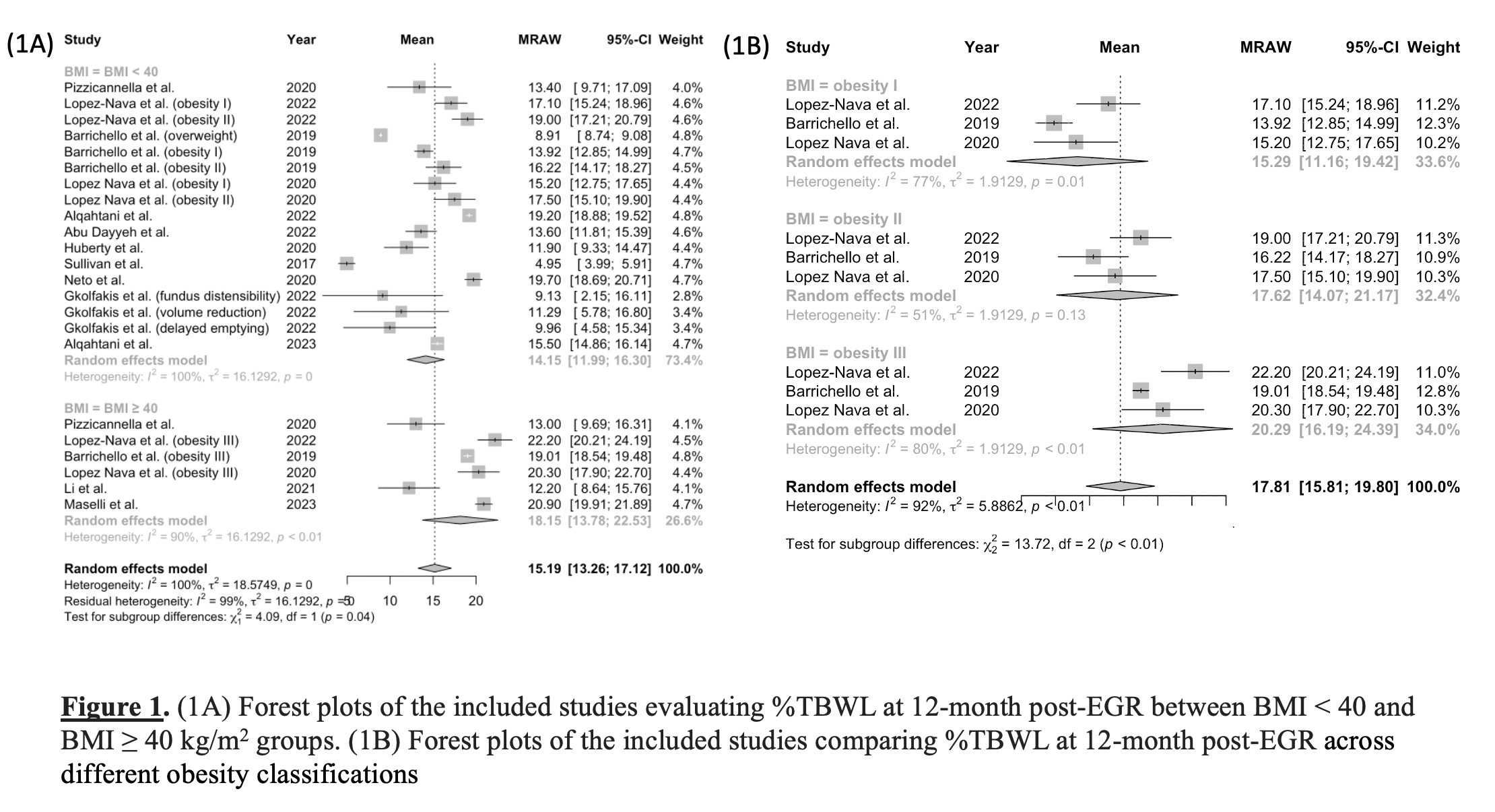
Figure: Figure 1. (1A) Forest plots of the included studies evaluating %TBWL at 12-month post-EGR between BMI < 40 and BMI ≥ 40 kg/m2 groups. (1B) Forest plots of the included studies comparing %TBWL at 12-month post-EGR across different obesity classifications
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Noppachai Siranart indicated no relevant financial relationships.
Christopher Thompson: Apollo Endosurgery – Consultant, Grant/Research Support. Bariendo – Consultant, Founder, Owner/Ownership Interest. Boston Scientific – Consultant, Grant/Research Support. Endoquest Robotics – Advisory Committee/Board Member, Consultant, Grant/Research Support. Endosim – Royalties. Enterasense Ltd. – Advisory Committee/Board Member, Consultant, Founder, Owner/Ownership Interest, Stock Options. EnVision Endoscopy – Advisory Committee/Board Member, Consultant, Founder, Owner/Ownership Interest, Stock Options. ERBE – Grant/Research Support. Fractyl – Consultant, Grant/Research Support, Stock Options. Fujifilm – Grant/Research Support. GI Dynamics – Consultant, Grant/Research Support. GI Windows – Advisory Committee/Board Member, Consultant, Founder, Owner/Ownership Interest, Royalties, Stock Options. Lumendi – Grant/Research Support. Medtronic – Advisory Committee/Board Member, Consultant. Olympus – Consultant, Grant/Research Support. USGI Medical – Advisory Committee/Board Member, Consultant, Grant/Research Support. Xenter – Advisory Committee/Board Member, Consultant.
Pichamol Jirapinyo: Apollo Endosurgery – Consultant, Grant/Research Support. Bariendo – Advisory Committee/Board Member, Consultant, Owner/Ownership Interest. Boston Scientific – Consultant, Grant/Research Support. Cook Medical – Consultant. Endosim – Royalties. ERBE – Consultant. Fractyl – Consultant, Grant/Research Support. GI Dynamics – Consultant, Grant/Research Support. Madrigal – Consultant. Spatz – Consultant. USGI Medical – Consultant, Grant/Research Support.
Noppachai Siranart, MD1, Christopher C.. Thompson, MD, MSc2, Pichamol Jirapinyo, MD, MPH3. P4884 - Weight Loss Outcomes in High BMI Patients After Endoscopic Gastric Remodeling: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
