Tuesday Poster Session
Category: Obesity
P4890 - Longitudinal Weight Loss Outcomes Following Transoral Outlet Reduction (TORe) in a Minority Patient Population at an Urban Safety Net Hospital
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- LK
Leah Kim, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Leah Kim, MD1, Abraham Z. Cheloff, MD, MS1, Manish Parikh, MD1, Rabia De Latour, MD2
1NYU Langone Health, New York, NY; 2NYU Grossman School of Medicine, New York, NY
Introduction: Transoral outlet reduction (TORe) is an endoscopic procedure that tightens the gastrojejunal anastomosis (GJA) of patients experiencing weight recidivism following Roux-en-Y gastric bypass (RYGB) surgery. Successful TORe outcomes have been demonstrated previously within higher resourced settings. Our goal is to evaluate longitudinal weight loss outcomes following TORe in a minority underserved population at an urban safety net hospital.
Methods: Retrospective review was performed to identify patients receiving TORe between 2018-2023. All patients had received prior RYGB and had experienced subsequent weight recidivism, with body mass index (BMI) >30 at time of TORe. Baseline demographics, baseline BMIs (at RYGB, at nadir after RYGB, at TORe), and time in years from RYGB to TORe were collected. Weight and BMI were tracked over time (at TORe; 6-, 12-, and 18-months after TORe) and were used to calculate % total body weight loss (% TBWL) and % excess body weight loss (% EBWL).
Results: Adequate follow-up data was available for 61 of the hundreds of patients who underwent TORe between 2018-2023. Of these 61 patients, 56 had 6-month data, 33 had 12-month data, and 23 had 18-month data. Sample characteristics were notable for a majority-minority population (62.3% Hispanic, 19.7% Black, 13.1% Multiracial or other, 4.9% White).
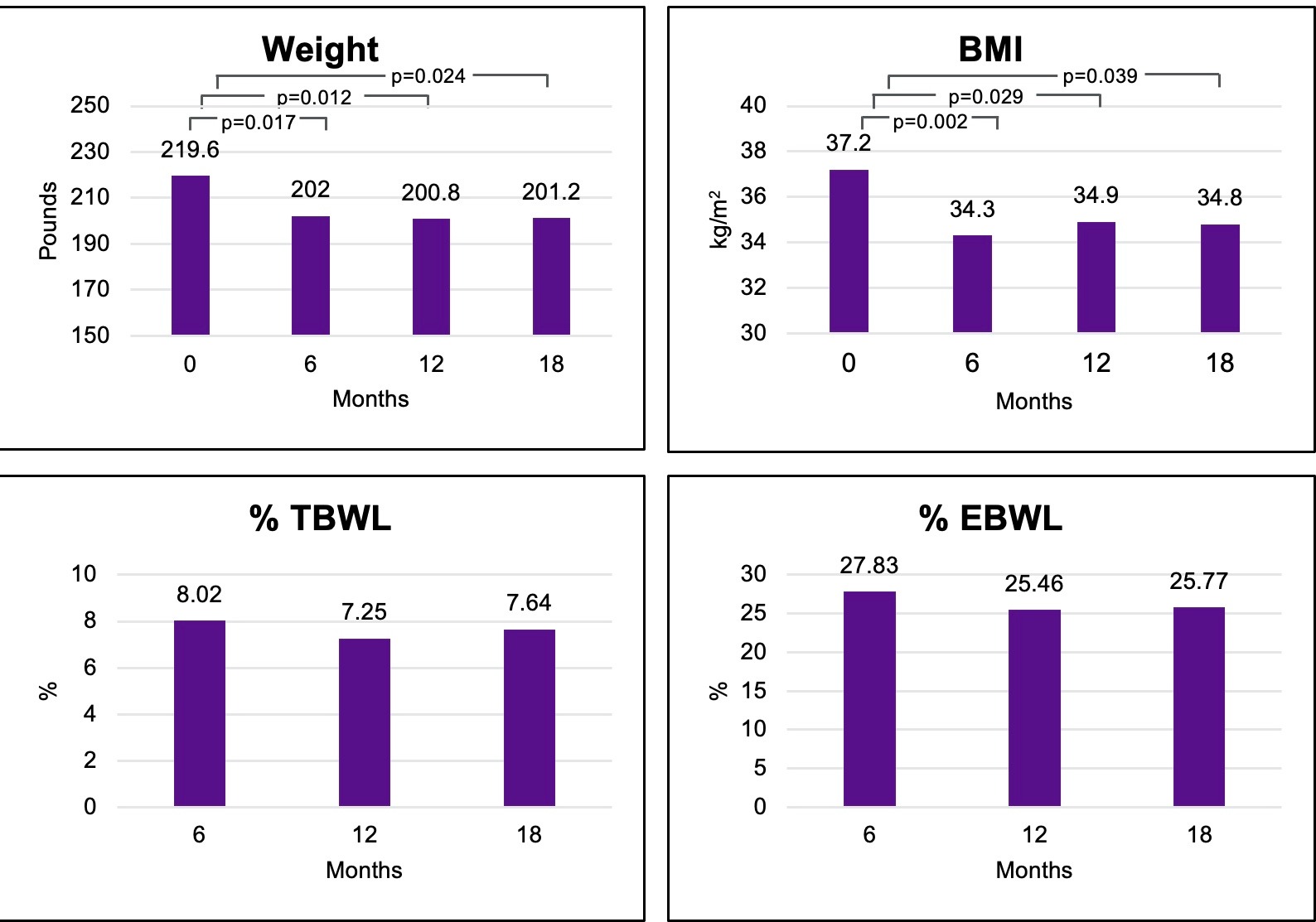
Mean weight at TORe was 219.6 ± 43.5 lbs, and there was significant sustained weight loss at 6-, 12-, and 18-months following TORe (202.0 ± 45.2 lbs, 200.8 ± 33.7 lbs, 201.2 ± 34.3 lbs; p< 0.05) when compared to baseline. Mean BMI at TORe was 37.2 ± 5.2 kg/m2, and BMI also demonstrated significant reduction at 6-, 12-, and 18-months (34.3 ± 5.6 kg/m2, 34.9 ± 5.9 kg/m2, 34.8 ± 5.6 kg/m2; p< 0.05). Additionally, at 6-, 12-, and 18-months, % TBWL (8.0%, 7.3%, 7.6%) and % EBWL (27.8%, 25.5%, 25.8%) were sustained.
Discussion: In a predominantly minority, underserved patient population receiving TORe at a resource limited institution, weight loss was significant and sustained over time, with outcomes comparable to prior established studies in higher resourced patient populations. Resource limitation, including absence of nutrition services available likely limited weight loss outcomes. Future directions include studying the cohort over more time, identifying unique barriers these patients may face in weight loss and maintenance, and working to improve resources in underserved areas to improve health outcomes in vulnerable, underserved populations.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Leah Kim, MD1, Abraham Z. Cheloff, MD, MS1, Manish Parikh, MD1, Rabia De Latour, MD2. P4890 - Longitudinal Weight Loss Outcomes Following Transoral Outlet Reduction (TORe) in a Minority Patient Population at an Urban Safety Net Hospital, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1NYU Langone Health, New York, NY; 2NYU Grossman School of Medicine, New York, NY
Introduction: Transoral outlet reduction (TORe) is an endoscopic procedure that tightens the gastrojejunal anastomosis (GJA) of patients experiencing weight recidivism following Roux-en-Y gastric bypass (RYGB) surgery. Successful TORe outcomes have been demonstrated previously within higher resourced settings. Our goal is to evaluate longitudinal weight loss outcomes following TORe in a minority underserved population at an urban safety net hospital.
Methods: Retrospective review was performed to identify patients receiving TORe between 2018-2023. All patients had received prior RYGB and had experienced subsequent weight recidivism, with body mass index (BMI) >30 at time of TORe. Baseline demographics, baseline BMIs (at RYGB, at nadir after RYGB, at TORe), and time in years from RYGB to TORe were collected. Weight and BMI were tracked over time (at TORe; 6-, 12-, and 18-months after TORe) and were used to calculate % total body weight loss (% TBWL) and % excess body weight loss (% EBWL).
Results: Adequate follow-up data was available for 61 of the hundreds of patients who underwent TORe between 2018-2023. Of these 61 patients, 56 had 6-month data, 33 had 12-month data, and 23 had 18-month data. Sample characteristics were notable for a majority-minority population (62.3% Hispanic, 19.7% Black, 13.1% Multiracial or other, 4.9% White).
Mean weight at TORe was 219.6 ± 43.5 lbs, and there was significant sustained weight loss at 6-, 12-, and 18-months following TORe (202.0 ± 45.2 lbs, 200.8 ± 33.7 lbs, 201.2 ± 34.3 lbs; p< 0.05) when compared to baseline. Mean BMI at TORe was 37.2 ± 5.2 kg/m2, and BMI also demonstrated significant reduction at 6-, 12-, and 18-months (34.3 ± 5.6 kg/m2, 34.9 ± 5.9 kg/m2, 34.8 ± 5.6 kg/m2; p< 0.05). Additionally, at 6-, 12-, and 18-months, % TBWL (8.0%, 7.3%, 7.6%) and % EBWL (27.8%, 25.5%, 25.8%) were sustained.
Discussion: In a predominantly minority, underserved patient population receiving TORe at a resource limited institution, weight loss was significant and sustained over time, with outcomes comparable to prior established studies in higher resourced patient populations. Resource limitation, including absence of nutrition services available likely limited weight loss outcomes. Future directions include studying the cohort over more time, identifying unique barriers these patients may face in weight loss and maintenance, and working to improve resources in underserved areas to improve health outcomes in vulnerable, underserved populations.
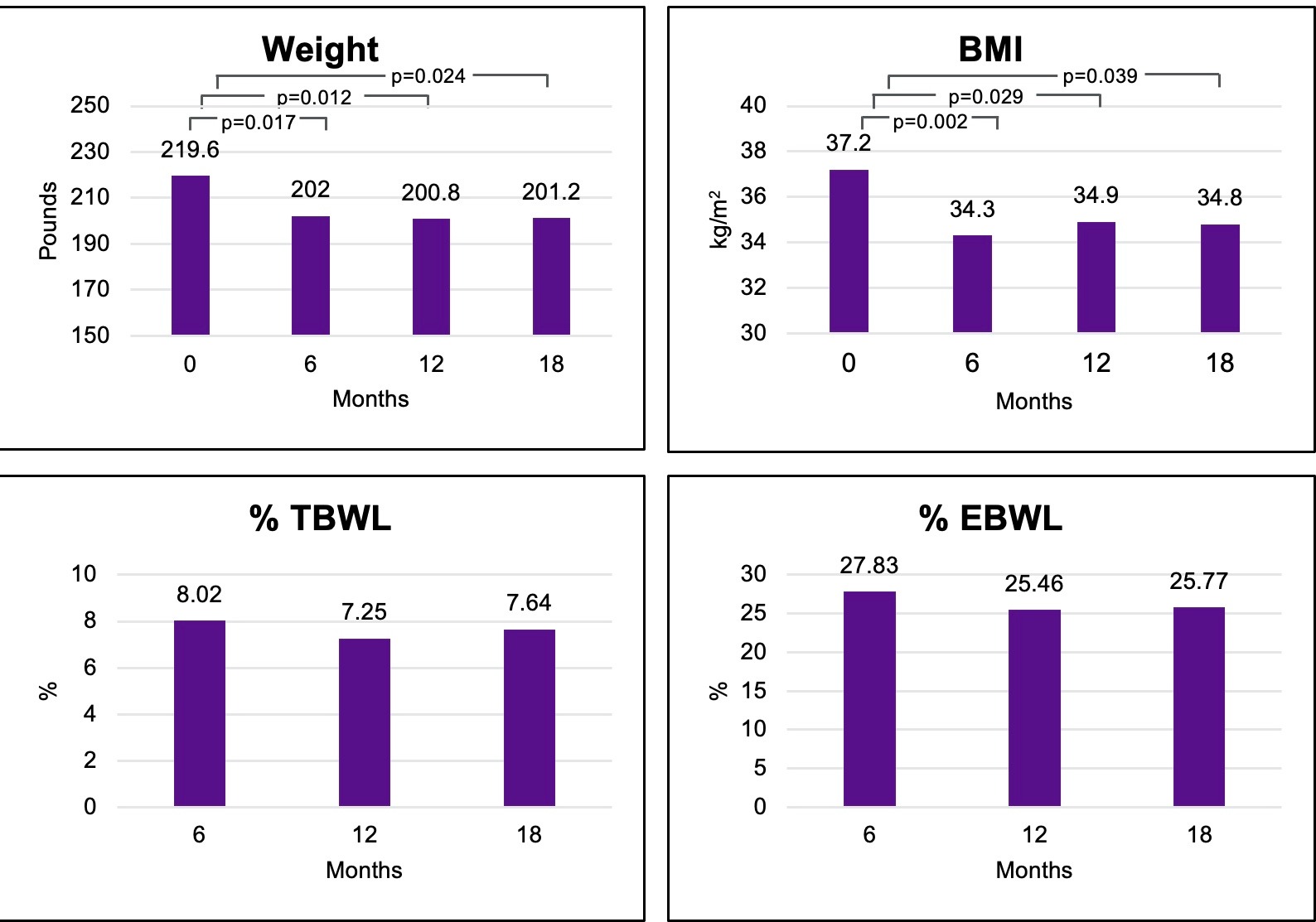
Figure: Figure 1: Weight, BMI, and weight loss markers at 6-, 12-, and 18-months following TORe.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Leah Kim indicated no relevant financial relationships.
Abraham Cheloff indicated no relevant financial relationships.
Manish Parikh indicated no relevant financial relationships.
Rabia De Latour: Boston Sci – Speakers Bureau.
Leah Kim, MD1, Abraham Z. Cheloff, MD, MS1, Manish Parikh, MD1, Rabia De Latour, MD2. P4890 - Longitudinal Weight Loss Outcomes Following Transoral Outlet Reduction (TORe) in a Minority Patient Population at an Urban Safety Net Hospital, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
