Tuesday Poster Session
Category: Practice Management
P4924 - Unveiling the COVID-19 Impact: Surging GI Disorders in Elderly Hospital Admissions
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MN
Mahum Nadeem, MBBS
Virginia Commonwealth University Health System
Henrico, VA
Presenting Author(s)
Mahum Nadeem, MBBS1, Apoorv Sharma, MS2, Richard Sterling, MD3, Ravi Vachhani, MD3
1Virginia Commonwealth University Health System, Henrico, VA; 2Virginia Commonwealth University, Charlottesville, VA; 3Virginia Commonwealth University Health System, Richmond, VA
Introduction: The burden of gastrointestinal (GI) disorders among the elderly, is substantial. The coronavirus disease 2019 (COVID-19) pandemic has reshaped healthcare delivery worldwide, impacting the management and outcomes of various medical conditions, including GI diseases. Our aim was to evaluate the impact of COVID-19 on GI-related hospital admissions among the older adults pre and post-pandemic to provide insights into the evolving landscape of GI healthcare
Methods: De-identified patient data from TriNetX was used to create 4 cohorts: pre-COVID (2016-2019) and post-COVID (2020-2023) for the 80–89 (Group A) and 90+ age group (Group B). Patients with primary GI diagnoses were identified using ICD-10 codes. Comparative analytics between Pre- and Post-COVID cohorts was used to examine demographic differences and the top GI diagnoses for each age group. Survival analysis was conducted using R's Survival packages and TriNetX analytics tools, including Measures of Association tests, Kaplan-Meier analysis, and Log-Rank tests to assess significant differences in one-year survival rates
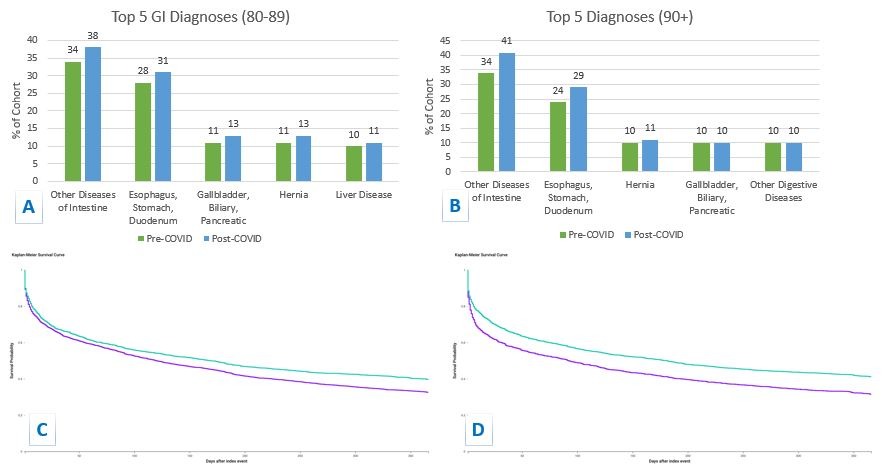
Results: The study included 15,520 patients, with 6870 (44%) in the pre-COVID period and 8650 (56%) in the post-COVID period, indicating a higher prevalence post-COVID. Female, Caucasian patients were the most common across both cohorts, followed by African Americans. Top 5 most common ICD 10 diagnosis of GI admissions included: diseases of intestine (A: 34 vs 38%, B: 34 vs 41%), diseases of stomach esophagus duodenum (A:28 vs 31%, B:24 vs 29%), hernia (A:11 vs 13%, B:10 vs 11%), disorders of biliary tract gallbladder and pancreas (A:11% vs 13%, B: 10% vs 10%) (Table & Figure 1A, 1B). Measures of association tests showed a higher relative risk of GI diseases post-COVID in both age groups: Group A (54 vs 59%, OR 1.21, CI: 1.11-1.32) and Group B (52 vs 59.%, OR 1.33, CI: 1.20-1.47), p< 0.0001. Kaplan-Meier analysis revealed lower 1-year survival rates in both post-COVID groups (A: 32 vs 39%, B: 41 vs 31%), p< 0.0001 (Figure 1C, 1D).
Discussion: Our study reveals a trend of increased prevalence and decreased survival rates among elderly pts with primary hospital admissions for gastrointestinal disorders post-COVID. With aging certain biological factors, such as decline of immune function, disrupted gut microbiota, modify susceptibility to gastrointestinal disorders. Delays and disruption in elective/diagnostic procedures and direct effects of COVID on GI tract are some of the factors that may have contribute to observed increased in GI diseases during COVID
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mahum Nadeem, MBBS1, Apoorv Sharma, MS2, Richard Sterling, MD3, Ravi Vachhani, MD3. P4924 - Unveiling the COVID-19 Impact: Surging GI Disorders in Elderly Hospital Admissions, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Virginia Commonwealth University Health System, Henrico, VA; 2Virginia Commonwealth University, Charlottesville, VA; 3Virginia Commonwealth University Health System, Richmond, VA
Introduction: The burden of gastrointestinal (GI) disorders among the elderly, is substantial. The coronavirus disease 2019 (COVID-19) pandemic has reshaped healthcare delivery worldwide, impacting the management and outcomes of various medical conditions, including GI diseases. Our aim was to evaluate the impact of COVID-19 on GI-related hospital admissions among the older adults pre and post-pandemic to provide insights into the evolving landscape of GI healthcare
Methods: De-identified patient data from TriNetX was used to create 4 cohorts: pre-COVID (2016-2019) and post-COVID (2020-2023) for the 80–89 (Group A) and 90+ age group (Group B). Patients with primary GI diagnoses were identified using ICD-10 codes. Comparative analytics between Pre- and Post-COVID cohorts was used to examine demographic differences and the top GI diagnoses for each age group. Survival analysis was conducted using R's Survival packages and TriNetX analytics tools, including Measures of Association tests, Kaplan-Meier analysis, and Log-Rank tests to assess significant differences in one-year survival rates
Results: The study included 15,520 patients, with 6870 (44%) in the pre-COVID period and 8650 (56%) in the post-COVID period, indicating a higher prevalence post-COVID. Female, Caucasian patients were the most common across both cohorts, followed by African Americans. Top 5 most common ICD 10 diagnosis of GI admissions included: diseases of intestine (A: 34 vs 38%, B: 34 vs 41%), diseases of stomach esophagus duodenum (A:28 vs 31%, B:24 vs 29%), hernia (A:11 vs 13%, B:10 vs 11%), disorders of biliary tract gallbladder and pancreas (A:11% vs 13%, B: 10% vs 10%) (Table & Figure 1A, 1B). Measures of association tests showed a higher relative risk of GI diseases post-COVID in both age groups: Group A (54 vs 59%, OR 1.21, CI: 1.11-1.32) and Group B (52 vs 59.%, OR 1.33, CI: 1.20-1.47), p< 0.0001. Kaplan-Meier analysis revealed lower 1-year survival rates in both post-COVID groups (A: 32 vs 39%, B: 41 vs 31%), p< 0.0001 (Figure 1C, 1D).
Discussion: Our study reveals a trend of increased prevalence and decreased survival rates among elderly pts with primary hospital admissions for gastrointestinal disorders post-COVID. With aging certain biological factors, such as decline of immune function, disrupted gut microbiota, modify susceptibility to gastrointestinal disorders. Delays and disruption in elective/diagnostic procedures and direct effects of COVID on GI tract are some of the factors that may have contribute to observed increased in GI diseases during COVID
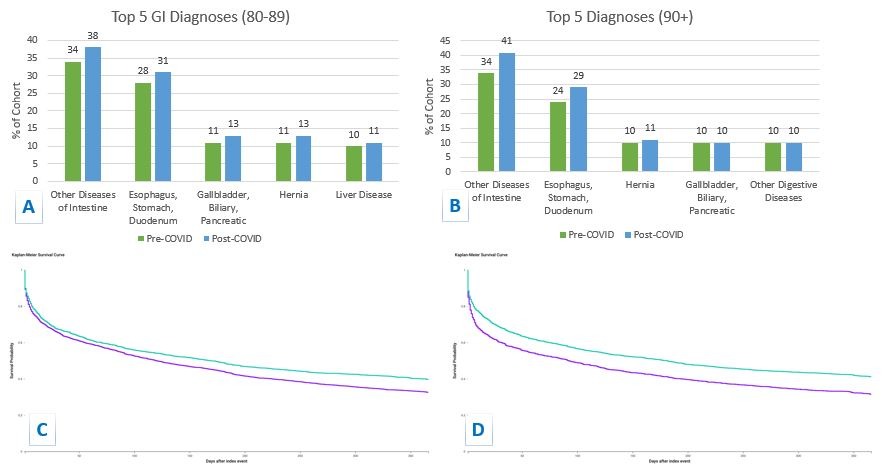
Figure: Figure A, B: Top 5 most common GI Diagnoses in Group A (Left top) and Group B (Right top), pre and post-COVID cohorts
Figure C, D: 1-year survival curves for Group A (Left bottom) and Group B (right bottom), pre and post-COVID cohorts
Figure C, D: 1-year survival curves for Group A (Left bottom) and Group B (right bottom), pre and post-COVID cohorts
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mahum Nadeem indicated no relevant financial relationships.
Apoorv Sharma indicated no relevant financial relationships.
Richard Sterling indicated no relevant financial relationships.
Ravi Vachhani indicated no relevant financial relationships.
Mahum Nadeem, MBBS1, Apoorv Sharma, MS2, Richard Sterling, MD3, Ravi Vachhani, MD3. P4924 - Unveiling the COVID-19 Impact: Surging GI Disorders in Elderly Hospital Admissions, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
