Tuesday Poster Session
Category: Practice Management
P4925 - The Value of EGD with EUS or ERCP: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- PY
Pradeep Yarra, MD
Saint Louis University School of Medicine
St. Louis, MO
Presenting Author(s)
Pradeep Yarra, MD1, Alexander J. Thomas, MD2, Bhavna Guduguntla, MD3, Karam Al-Bayati, MD4, Raj Shah, MD5, Thomas R.. McCarty, MD, MPH6, Ahmad Najdat Bazarbashi, MD7
1Saint Louis University School of Medicine, St. Louis, MO; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Washington University School of Medicine in St. Louis, St. Louis, MO; 4University of Manitoba, Winnipeg, MB, Canada; 5The Ohio State University Wexner Medical Center, Columbus, OH; 6Houston Methodist Hospital, Houston, TX; 7Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO
Introduction: Endoscopic ultrasonography (EUS) and endoscopic retrograde cholangiopancreaticography (ERCP) are common endoscopic procedures performed for the diagnosis and management of various gastrointestinal conditions. However, luminal or mucosal pathology may be missed due to the “side-viewer” nature of these endoscopes. Some endoscopists advocate for the use of standard forward-view prior to EUS/ERCP to evaluate for clinically significant pathology. Our aim was to evaluate the clinical utility and efficacy of EGD before or after EUS/ERCP through a systematic review and meta-analysis.
Methods: Following PRISMA and MOOSE guidelines, a systematic review was conducted in PubMed, EMBASE, Cochrane and Web of Science from inception to date for identifying studies on outcomes of EGD before or after EUS/ERCP. Search strategy was performed with the aid of a librarian. The primary outcome was pooled number/percentage of lesions noted on EGD which would have been otherwise missed on EUS. Secondary outcomes are clinically significant lesions as defined in relevant studies and number of missed lesions. Pooled estimates were calculated using a random effects model with 95% confidence interval (CI). Heterogeneity was assessed with
I2 statistics and Q testing. Publication bias was assessed via visually inspected for asymmetry and quantitatively assessed using Egger regression testing.
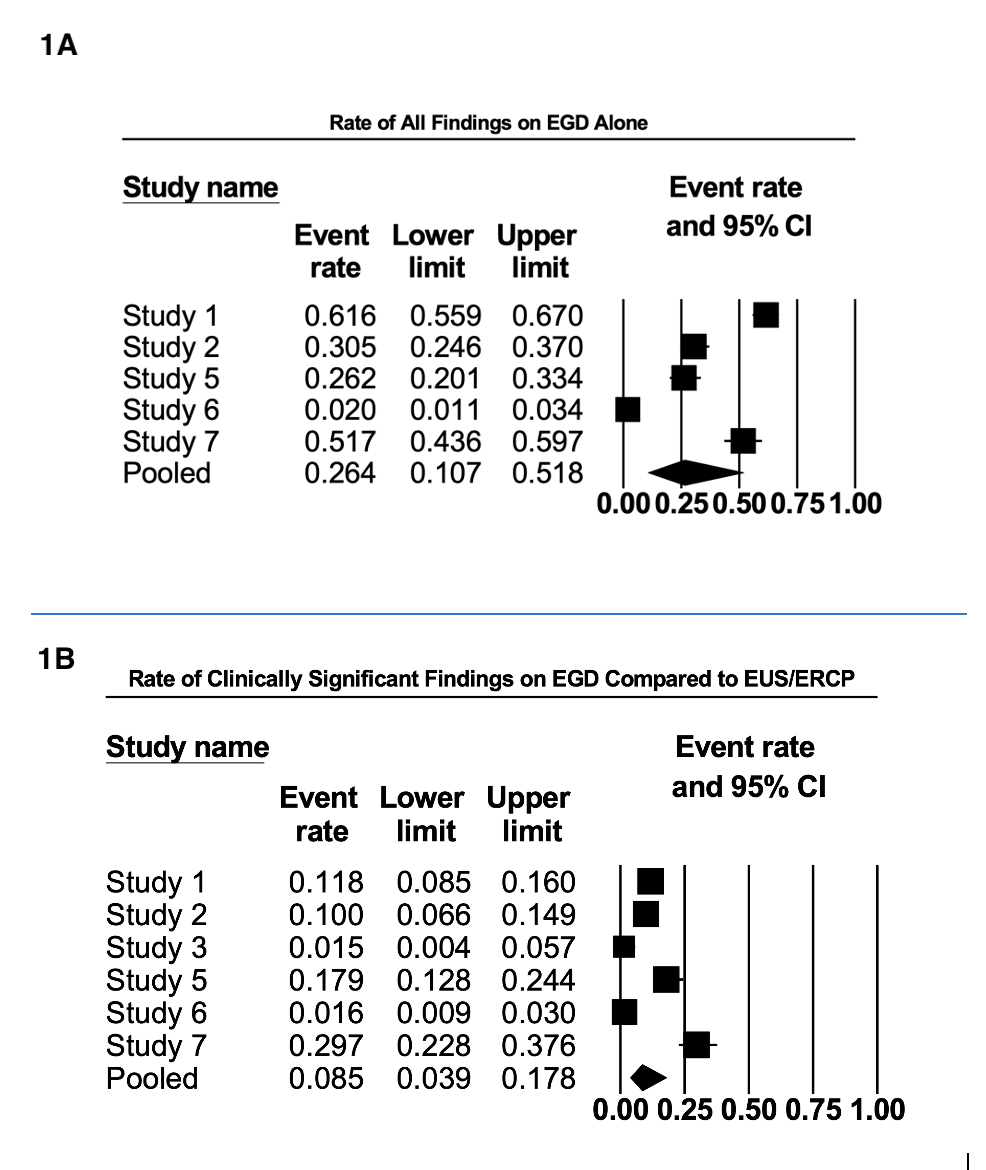
Results: A total of 7 studies (n=1737 patients) were included in this analysis. Four studies were retrospective, two studies were prospective, and one study was a tandem prospective, blinded trial. Mean age of included patients was 68.87 (57-71) years, with 50.02% female. The rate of all findings detected on EGD alone was 20.01% [(95% CI, 9.16-38.28); I<sup>2</sup>=97.74; Q-value 265.30] – (Figure 1A). In total, forward viewing EGD found more lesions than EUS or ERCP at a rate of 9.68% [(95% CI, 4.17-20.90); I<sup>2</sup>=96.50; Q-value 171.51]. A total of 6 studies (n=1562) examined difference in clinically significant findings, defined as those that required change in management. These were noted for 8.54% [(95% CI, 3.86-17.82); I<sup>2</sup>=94.78; Q-value 85.87] of patients – (Figure 1B). There was no evidence of publication bias.
Discussion: EGD with EUS or ERCP routinely diagnoses clinically significant pathology that may be otherwise missed and therefore should be performed with each EUS and ERCP routinely.
Disclosures:
Pradeep Yarra, MD1, Alexander J. Thomas, MD2, Bhavna Guduguntla, MD3, Karam Al-Bayati, MD4, Raj Shah, MD5, Thomas R.. McCarty, MD, MPH6, Ahmad Najdat Bazarbashi, MD7. P4925 - The Value of EGD with EUS or ERCP: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Louis University School of Medicine, St. Louis, MO; 2SSM Health Saint Louis University Hospital, St. Louis, MO; 3Washington University School of Medicine in St. Louis, St. Louis, MO; 4University of Manitoba, Winnipeg, MB, Canada; 5The Ohio State University Wexner Medical Center, Columbus, OH; 6Houston Methodist Hospital, Houston, TX; 7Washington University School of Medicine in St. Louis / Barnes-Jewish Hospital, St. Louis, MO
Introduction: Endoscopic ultrasonography (EUS) and endoscopic retrograde cholangiopancreaticography (ERCP) are common endoscopic procedures performed for the diagnosis and management of various gastrointestinal conditions. However, luminal or mucosal pathology may be missed due to the “side-viewer” nature of these endoscopes. Some endoscopists advocate for the use of standard forward-view prior to EUS/ERCP to evaluate for clinically significant pathology. Our aim was to evaluate the clinical utility and efficacy of EGD before or after EUS/ERCP through a systematic review and meta-analysis.
Methods: Following PRISMA and MOOSE guidelines, a systematic review was conducted in PubMed, EMBASE, Cochrane and Web of Science from inception to date for identifying studies on outcomes of EGD before or after EUS/ERCP. Search strategy was performed with the aid of a librarian. The primary outcome was pooled number/percentage of lesions noted on EGD which would have been otherwise missed on EUS. Secondary outcomes are clinically significant lesions as defined in relevant studies and number of missed lesions. Pooled estimates were calculated using a random effects model with 95% confidence interval (CI). Heterogeneity was assessed with
I2 statistics and Q testing. Publication bias was assessed via visually inspected for asymmetry and quantitatively assessed using Egger regression testing.
Results: A total of 7 studies (n=1737 patients) were included in this analysis. Four studies were retrospective, two studies were prospective, and one study was a tandem prospective, blinded trial. Mean age of included patients was 68.87 (57-71) years, with 50.02% female. The rate of all findings detected on EGD alone was 20.01% [(95% CI, 9.16-38.28); I<sup>2</sup>=97.74; Q-value 265.30] – (Figure 1A). In total, forward viewing EGD found more lesions than EUS or ERCP at a rate of 9.68% [(95% CI, 4.17-20.90); I<sup>2</sup>=96.50; Q-value 171.51]. A total of 6 studies (n=1562) examined difference in clinically significant findings, defined as those that required change in management. These were noted for 8.54% [(95% CI, 3.86-17.82); I<sup>2</sup>=94.78; Q-value 85.87] of patients – (Figure 1B). There was no evidence of publication bias.
Discussion: EGD with EUS or ERCP routinely diagnoses clinically significant pathology that may be otherwise missed and therefore should be performed with each EUS and ERCP routinely.
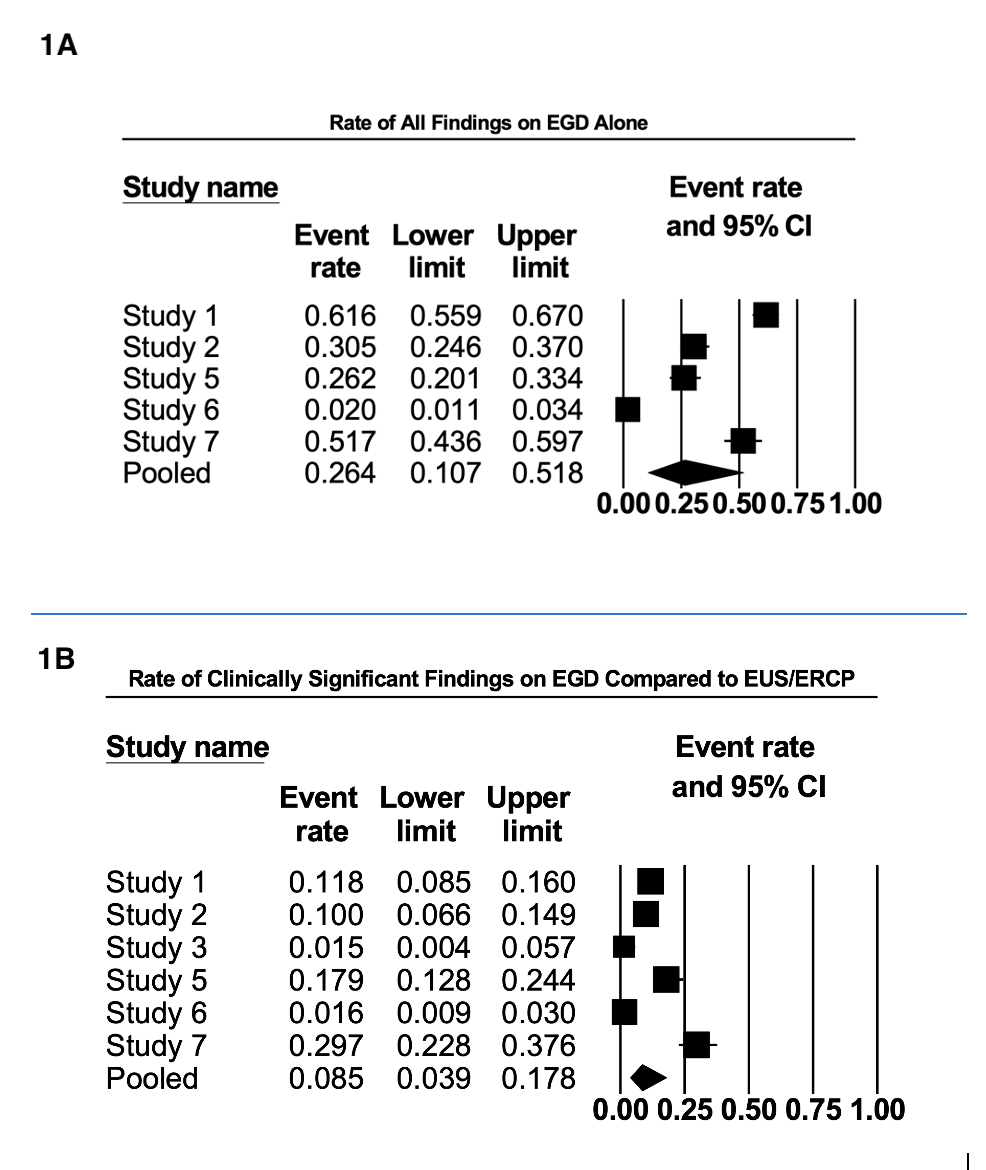
Figure: Figure 1A: Rate of all Findings on EGD Alone
Figure 1B: Rate of Clinically Significant Findings on EGD Compared to EUS/ERCP
Figure 1B: Rate of Clinically Significant Findings on EGD Compared to EUS/ERCP
Disclosures:
Pradeep Yarra indicated no relevant financial relationships.
Alexander Thomas indicated no relevant financial relationships.
Bhavna Guduguntla indicated no relevant financial relationships.
Karam Al-Bayati indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Thomas McCarty indicated no relevant financial relationships.
Ahmad Najdat Bazarbashi indicated no relevant financial relationships.
Pradeep Yarra, MD1, Alexander J. Thomas, MD2, Bhavna Guduguntla, MD3, Karam Al-Bayati, MD4, Raj Shah, MD5, Thomas R.. McCarty, MD, MPH6, Ahmad Najdat Bazarbashi, MD7. P4925 - The Value of EGD with EUS or ERCP: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
