Tuesday Poster Session
Category: Small Intestine
P4940 - Race and Gender-Based Differences in Healthcare Utilization for Common Gastrointestinal Symptoms Among Veterans
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MP
Mansour Parsi, MD, MPH, MBA.
University of Tennessee College of Medicine
Memphis, TN
Presenting Author(s)
Mansour Parsi, MD, MPH, MBA.1, QiQi Zhou, MD, PhD1, Leonard Baidoo, MD1, Yu Jiang, PhD.2, G. Nicholas Verne, MD1
1University of Tennessee College of Medicine, Memphis, TN; 2University of Memphis, Memphis, TN
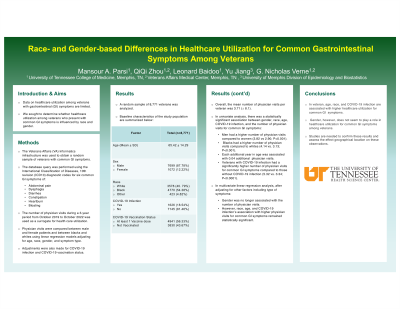
Introduction: Timely diagnosis and treatment are crucial for favorable disease outcomes and are influenced by healthcare utilization. Data on healthcare utilization among patients with gastrointestinal (GI) symptoms are limited, particularly in veteran populations. We aimed to determine whether healthcare utilization among veterans presenting with common GI symptoms is influenced by race and gender.
Methods: The U.S. Department of Veterans Affairs’ electronic healthcare database was used to obtain a random sample of veterans with common GI symptoms. The database query was performed utilizing the International Classification of Diseases, 10th revision (ICD10) diagnostic codes for six common GI symptoms including abdominal pain, dysphagia, diarrhea, constipation, heartburn, and bloating. The number of physician visits during a 3-year period from October 2019 to October 2022 was used as a surrogate for health care utilization. Physician visits were compared between male and female patients and between blacks and whites using linear regression models adjusting for age, race, gender, and symptom type. Adjustments were also made for COVID-19 infection and COVID-19 vaccination status.
Results: A random sample of 8,771 veterans was analyzed. Baseline characteristics of the study cohort are summarized in Table 1. Overall, the mean number of physician visits per veteran was 3.71 (± 8.1). In univariate analysis, there was a statistically significant association between gender, race, age, COVID-19 infection, and the number of physician visits for common GI symptoms. Men had a higher number of physician visits compared to women (3.82 vs 2.90; P< 0.001) and blacks had a higher number of physician visits compared to whites (4.14 vs. 3.13; P< 0.001). On average, each additional year in age was associated with 0.04 additional physician visits. Veterans with COVID-19 infection had a significantly higher number of physician visits for common GI symptoms compared to those without COVID-19 infection (5.32 vs. 3.34; P< 0.0001). In multivariate linear regression analysis, after adjusting for other factors including type of symptoms, gender was not associated with the number of physician visits but race, age, and COVID-19 infection’s association with higher physician visits remained statistically significant.
Discussion: In veterans, age, race, and COVID-19 infection are associated with higher healthcare utilization for common GI symptoms while gender does not seem to play a role after adjusting for other factors.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mansour Parsi, MD, MPH, MBA.1, QiQi Zhou, MD, PhD1, Leonard Baidoo, MD1, Yu Jiang, PhD.2, G. Nicholas Verne, MD1. P4940 - Race and Gender-Based Differences in Healthcare Utilization for Common Gastrointestinal Symptoms Among Veterans, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Tennessee College of Medicine, Memphis, TN; 2University of Memphis, Memphis, TN
Introduction: Timely diagnosis and treatment are crucial for favorable disease outcomes and are influenced by healthcare utilization. Data on healthcare utilization among patients with gastrointestinal (GI) symptoms are limited, particularly in veteran populations. We aimed to determine whether healthcare utilization among veterans presenting with common GI symptoms is influenced by race and gender.
Methods: The U.S. Department of Veterans Affairs’ electronic healthcare database was used to obtain a random sample of veterans with common GI symptoms. The database query was performed utilizing the International Classification of Diseases, 10th revision (ICD10) diagnostic codes for six common GI symptoms including abdominal pain, dysphagia, diarrhea, constipation, heartburn, and bloating. The number of physician visits during a 3-year period from October 2019 to October 2022 was used as a surrogate for health care utilization. Physician visits were compared between male and female patients and between blacks and whites using linear regression models adjusting for age, race, gender, and symptom type. Adjustments were also made for COVID-19 infection and COVID-19 vaccination status.
Results: A random sample of 8,771 veterans was analyzed. Baseline characteristics of the study cohort are summarized in Table 1. Overall, the mean number of physician visits per veteran was 3.71 (± 8.1). In univariate analysis, there was a statistically significant association between gender, race, age, COVID-19 infection, and the number of physician visits for common GI symptoms. Men had a higher number of physician visits compared to women (3.82 vs 2.90; P< 0.001) and blacks had a higher number of physician visits compared to whites (4.14 vs. 3.13; P< 0.001). On average, each additional year in age was associated with 0.04 additional physician visits. Veterans with COVID-19 infection had a significantly higher number of physician visits for common GI symptoms compared to those without COVID-19 infection (5.32 vs. 3.34; P< 0.0001). In multivariate linear regression analysis, after adjusting for other factors including type of symptoms, gender was not associated with the number of physician visits but race, age, and COVID-19 infection’s association with higher physician visits remained statistically significant.
Discussion: In veterans, age, race, and COVID-19 infection are associated with higher healthcare utilization for common GI symptoms while gender does not seem to play a role after adjusting for other factors.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mansour Parsi indicated no relevant financial relationships.
QiQi Zhou indicated no relevant financial relationships.
Leonard Baidoo: Bristol Myers Sqibb – Speakers Bureau. Pfizer – Speakers Bureau.
Yu Jiang indicated no relevant financial relationships.
G. Nicholas Verne indicated no relevant financial relationships.
Mansour Parsi, MD, MPH, MBA.1, QiQi Zhou, MD, PhD1, Leonard Baidoo, MD1, Yu Jiang, PhD.2, G. Nicholas Verne, MD1. P4940 - Race and Gender-Based Differences in Healthcare Utilization for Common Gastrointestinal Symptoms Among Veterans, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
