Tuesday Poster Session
Category: Small Intestine
P4942 - Recurrent Lymphoma in the Terminal Ileum
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- IR
Ibrahim Ragab, DO
St. Luke's University Hospital
Allentown, PA
Presenting Author(s)
Ibrahim Ragab, DO1, Bryan Wey, MD2, Kimberly Chaput, DO2
1St. Luke's University Hospital, Allentown, PA; 2St. Luke's University Health Network, Bethlehem, PA
Introduction: Malignancy in the small bowel is rare, representing less than 5% of all gastrointestinal cancers. Lymphoma of the small bowel is one of the most common types of primary gastrointestinal lymphoma, with Diffuse large B-cell lymphoma (DLBCL) most often presenting in the terminal ileum due its abundance of lymphoid tissue. Its presentation can vary, often presenting with similar symptoms to other conditions such as Crohn’s disease, small bowel obstruction (SBO), or appendicitis. Diagnosis is established by a combination of imaging and biopsy samples. The management of small bowel lymphoma involves surgical resection followed by adjuvant chemotherapy and, in some cases, radiation therapy.
Case Description/Methods: Here we present a case of a 25-year-old male with a history of terminal ileal DLBCL diagnosed ten years prior, which was treated with partial small bowel resection and adjuvant chemotherapy. Exploratory laparotomy a year later was performed for recurrent distal SBO, where he underwent additional small bowel resection and biopsy of two nearby lymph nodes. Pathology showed extensive, transmural granulomatous inflammation without recurrence of lymphoma, and flow cytometry was negative for a clonal B cell population. Surveillance colonoscopy several years later showed a grossly normal terminal ileum, with no evidence of residual lymphoma. However, he soon developed a perianal fistula with biopsies showing active inflammation despite his biomarkers not being suggestive of Crohn’s disease.
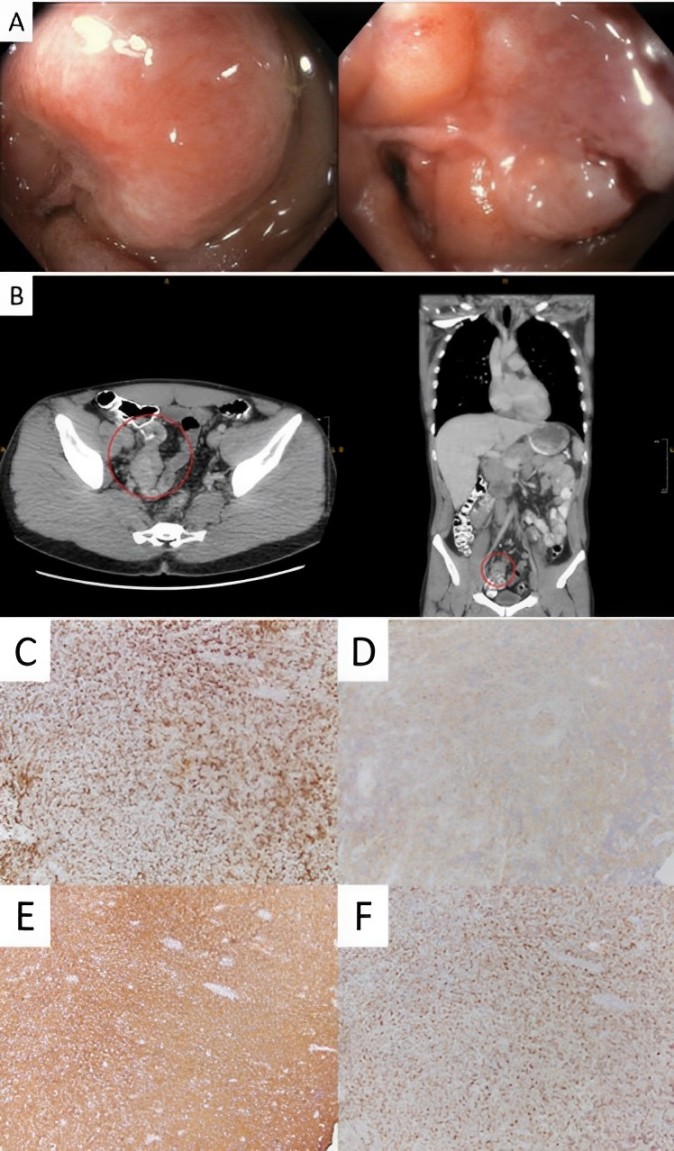
He had been doing well until he developed epigastric pain that persisted for a few months without any dysphagia, dyspepsia, hematemesis, melena, right upper quadrant pain, NSAID use, excessive alcohol use, or B symptoms. CT scan showed mural thickening of the terminal ileum and colonoscopy revealed abnormal mucosa in the terminal ileum. Biopsies ultimately revealed a prominent infiltrate of large, atypical lymphocytes. Immunohistochemical staining identified these cells as CD20 positive B cells, suggestive of recurrent/residual disease. He was referred to surgical oncology and medical oncology for additional management.
Discussion: The presentation of DLBCL in the terminal ileum highlights the importance of considering a broad differential diagnosis when encountering nonspecific gastrointestinal symptoms. The combination of imaging, endoscopy, and biopsy samples is essential in making an accurate diagnosis.
Disclosures:
Ibrahim Ragab, DO1, Bryan Wey, MD2, Kimberly Chaput, DO2. P4942 - Recurrent Lymphoma in the Terminal Ileum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Luke's University Hospital, Allentown, PA; 2St. Luke's University Health Network, Bethlehem, PA
Introduction: Malignancy in the small bowel is rare, representing less than 5% of all gastrointestinal cancers. Lymphoma of the small bowel is one of the most common types of primary gastrointestinal lymphoma, with Diffuse large B-cell lymphoma (DLBCL) most often presenting in the terminal ileum due its abundance of lymphoid tissue. Its presentation can vary, often presenting with similar symptoms to other conditions such as Crohn’s disease, small bowel obstruction (SBO), or appendicitis. Diagnosis is established by a combination of imaging and biopsy samples. The management of small bowel lymphoma involves surgical resection followed by adjuvant chemotherapy and, in some cases, radiation therapy.
Case Description/Methods: Here we present a case of a 25-year-old male with a history of terminal ileal DLBCL diagnosed ten years prior, which was treated with partial small bowel resection and adjuvant chemotherapy. Exploratory laparotomy a year later was performed for recurrent distal SBO, where he underwent additional small bowel resection and biopsy of two nearby lymph nodes. Pathology showed extensive, transmural granulomatous inflammation without recurrence of lymphoma, and flow cytometry was negative for a clonal B cell population. Surveillance colonoscopy several years later showed a grossly normal terminal ileum, with no evidence of residual lymphoma. However, he soon developed a perianal fistula with biopsies showing active inflammation despite his biomarkers not being suggestive of Crohn’s disease.
He had been doing well until he developed epigastric pain that persisted for a few months without any dysphagia, dyspepsia, hematemesis, melena, right upper quadrant pain, NSAID use, excessive alcohol use, or B symptoms. CT scan showed mural thickening of the terminal ileum and colonoscopy revealed abnormal mucosa in the terminal ileum. Biopsies ultimately revealed a prominent infiltrate of large, atypical lymphocytes. Immunohistochemical staining identified these cells as CD20 positive B cells, suggestive of recurrent/residual disease. He was referred to surgical oncology and medical oncology for additional management.
Discussion: The presentation of DLBCL in the terminal ileum highlights the importance of considering a broad differential diagnosis when encountering nonspecific gastrointestinal symptoms. The combination of imaging, endoscopy, and biopsy samples is essential in making an accurate diagnosis.
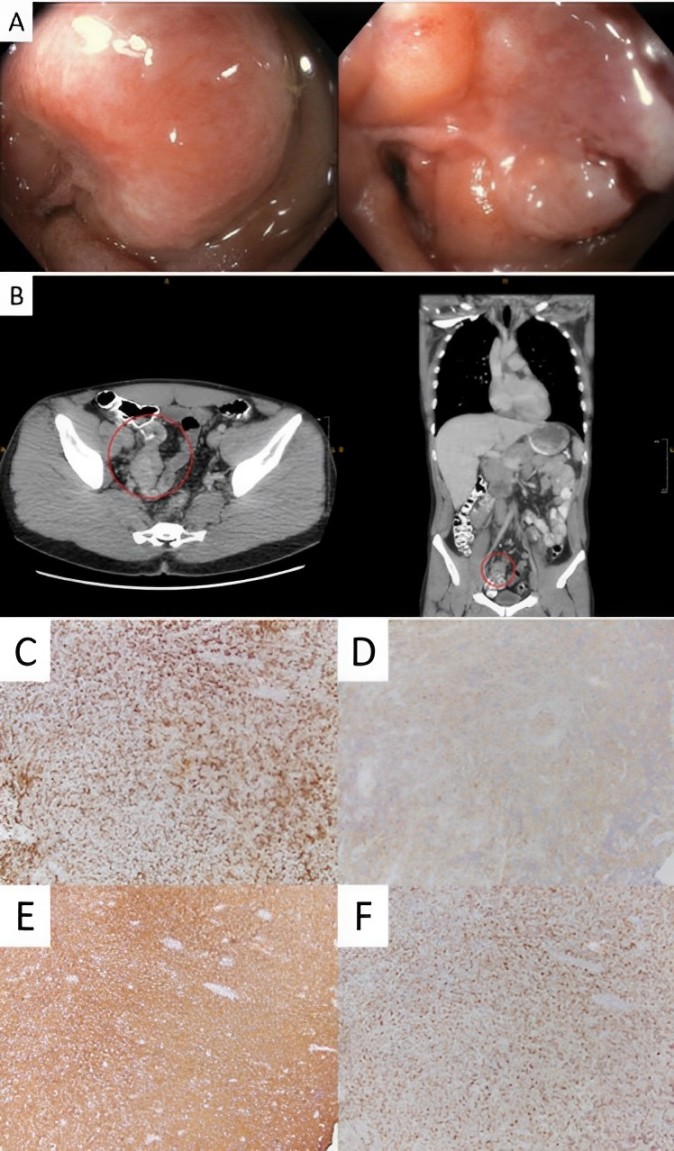
Figure: A. Abnormal mucosa at the terminal ileum
B. Terminal ileal wall thickening seen on contrast-enhanced CT
C. Histology of terminal ileal biopsies at 200x magnification with BCL6 staining
D. Histology of terminal ileal biopsies at 200x magnification with CD10 staining
E. Histology of terminal ileal biopsies at 200x magnification with CD20 staining
F. Histology of terminal ileal biopsies at 200x magnification with MUM1 staining
B. Terminal ileal wall thickening seen on contrast-enhanced CT
C. Histology of terminal ileal biopsies at 200x magnification with BCL6 staining
D. Histology of terminal ileal biopsies at 200x magnification with CD10 staining
E. Histology of terminal ileal biopsies at 200x magnification with CD20 staining
F. Histology of terminal ileal biopsies at 200x magnification with MUM1 staining
Disclosures:
Ibrahim Ragab indicated no relevant financial relationships.
Bryan Wey indicated no relevant financial relationships.
Kimberly Chaput indicated no relevant financial relationships.
Ibrahim Ragab, DO1, Bryan Wey, MD2, Kimberly Chaput, DO2. P4942 - Recurrent Lymphoma in the Terminal Ileum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
