Tuesday Poster Session
Category: Small Intestine
P4947 - When Eosinophils Invade: A Case of Eosinophilic Esophagitis and Gastroenteritis With Differential Responses to Therapy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Sarah Dwyer Holland, MD, MS
Brown University
Providence, RI
Presenting Author(s)
Sarah Dwyer Holland, MD, MS1, Wen Ting Yang, MD2, Nathan Sairam, MD2, Harlan Rich, MD2
1Brown University, Providence, RI; 2Brown University / Rhode Island Hospital, Providence, RI
Introduction: Eosinophilic gastrointestinal diseases can be difficult to manage. Recent reports have shown dupilumab may induce symptomatic and histologic remission of non-eosinophilic esophagitis eosinophilic gastrointestinal diseases (non-EOE EGID). We present a case of a patient with both eosinophilic esophagitis (EoE) and eosinophilic gastroenteritis. This patient’s symptoms related to eosinophilic esophagitis were refractory to standard therapy but improved after systemic steroids. However, his eosinophilic gastroenteritis was not controlled until the introduction of dupilumab.
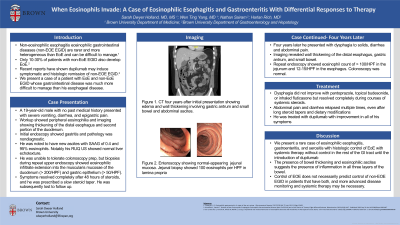
Case Description/Methods: A 19-year-old male with no past medical history presented with severe vomiting, diarrhea, and epigastric pain. Workup showed peripheral eosinophilia and imaging showing thickening of the distal esophagus and second portion of the duodenum. Initial endoscopy showed gastritis and pathology was nondiagnostic. He was noted to have new ascites with SAAG of 0.4 and 95% eosinophils.
He was unable to tolerate colonoscopy prep, but biopsies during repeat upper endoscopy showed eosinophilic infiltrate extension into the muscularis mucosae of the duodenum ( > 200/HPF) and gastric epithelium ( > 50/HPF). Symptoms resolved completely after 48 hours of steroids, and he was prescribed a slow steroid taper. He was subsequently lost to follow up.
Four years later he presented with dysphagia to solids, diarrhea and abdominal pain. Imaging revealed wall thickening of the distal esophagus and small bowel. His dysphagia did not improve with pantoprazole, topical budesonide, or inhaled fluticasone but resolved completely with systemic steroids. His gastrointestinal symptoms relapsed multiple times, even after long steroid tapers. Repeat endoscopy showed eosinophil count of > 100/HPF in the jejunum and 12-15/HPF in the esophagus. Colonoscopy was normal. Extensive workup with Hematology and Allergy/Immunology was unremarkable for any other explanation for peripheral eosinophilia. He was treated with dupilumab with improvement in his symptoms.
Discussion: We present a rare case of eosinophilic esophagitis, gastroenteritis, and serositis with histologic control of EoE with systemic therapy without control in the rest of the GI tract. The presence of thickening and ascites suggests the presence of inflammation in all three layers of the bowel. Control of EOE does not necessarily predict control of non-EOE EGID in patients that have both, and more advanced disease monitoring and systemic therapy may be necessary.
Disclosures:
Sarah Dwyer Holland, MD, MS1, Wen Ting Yang, MD2, Nathan Sairam, MD2, Harlan Rich, MD2. P4947 - When Eosinophils Invade: A Case of Eosinophilic Esophagitis and Gastroenteritis With Differential Responses to Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown University, Providence, RI; 2Brown University / Rhode Island Hospital, Providence, RI
Introduction: Eosinophilic gastrointestinal diseases can be difficult to manage. Recent reports have shown dupilumab may induce symptomatic and histologic remission of non-eosinophilic esophagitis eosinophilic gastrointestinal diseases (non-EOE EGID). We present a case of a patient with both eosinophilic esophagitis (EoE) and eosinophilic gastroenteritis. This patient’s symptoms related to eosinophilic esophagitis were refractory to standard therapy but improved after systemic steroids. However, his eosinophilic gastroenteritis was not controlled until the introduction of dupilumab.
Case Description/Methods: A 19-year-old male with no past medical history presented with severe vomiting, diarrhea, and epigastric pain. Workup showed peripheral eosinophilia and imaging showing thickening of the distal esophagus and second portion of the duodenum. Initial endoscopy showed gastritis and pathology was nondiagnostic. He was noted to have new ascites with SAAG of 0.4 and 95% eosinophils.
He was unable to tolerate colonoscopy prep, but biopsies during repeat upper endoscopy showed eosinophilic infiltrate extension into the muscularis mucosae of the duodenum ( > 200/HPF) and gastric epithelium ( > 50/HPF). Symptoms resolved completely after 48 hours of steroids, and he was prescribed a slow steroid taper. He was subsequently lost to follow up.
Four years later he presented with dysphagia to solids, diarrhea and abdominal pain. Imaging revealed wall thickening of the distal esophagus and small bowel. His dysphagia did not improve with pantoprazole, topical budesonide, or inhaled fluticasone but resolved completely with systemic steroids. His gastrointestinal symptoms relapsed multiple times, even after long steroid tapers. Repeat endoscopy showed eosinophil count of > 100/HPF in the jejunum and 12-15/HPF in the esophagus. Colonoscopy was normal. Extensive workup with Hematology and Allergy/Immunology was unremarkable for any other explanation for peripheral eosinophilia. He was treated with dupilumab with improvement in his symptoms.
Discussion: We present a rare case of eosinophilic esophagitis, gastroenteritis, and serositis with histologic control of EoE with systemic therapy without control in the rest of the GI tract. The presence of thickening and ascites suggests the presence of inflammation in all three layers of the bowel. Control of EOE does not necessarily predict control of non-EOE EGID in patients that have both, and more advanced disease monitoring and systemic therapy may be necessary.
Disclosures:
Sarah Dwyer Holland indicated no relevant financial relationships.
Wen Ting Yang indicated no relevant financial relationships.
Nathan Sairam indicated no relevant financial relationships.
Harlan Rich indicated no relevant financial relationships.
Sarah Dwyer Holland, MD, MS1, Wen Ting Yang, MD2, Nathan Sairam, MD2, Harlan Rich, MD2. P4947 - When Eosinophils Invade: A Case of Eosinophilic Esophagitis and Gastroenteritis With Differential Responses to Therapy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

