Tuesday Poster Session
Category: Small Intestine
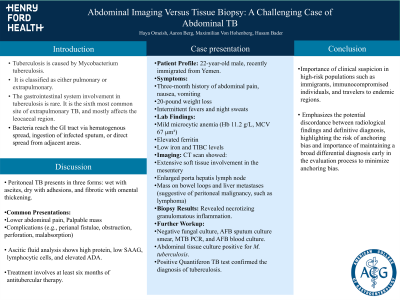
P4953 - Abdominal Imaging Versus Tissue Biopsy: A Challenging Case of Abdominal TB
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- HO
Haya Omeish, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Haya Omeish, MD1, Aaron Berg, MD2, Maximilian Von Hohenberg, MD2, Husam Bader, MD2
1Henry Ford Health, Detroit, MI; 2University of Michigan, Ann Arbor, MI
Introduction: Tuberculosis, caused by Mycobacterium tuberculosis, remains one of the leading infectious causes of death worldwide. It is classified as either pulmonary or extrapulmonary. The gastrointestinal system involvement in tuberculosis is rare.
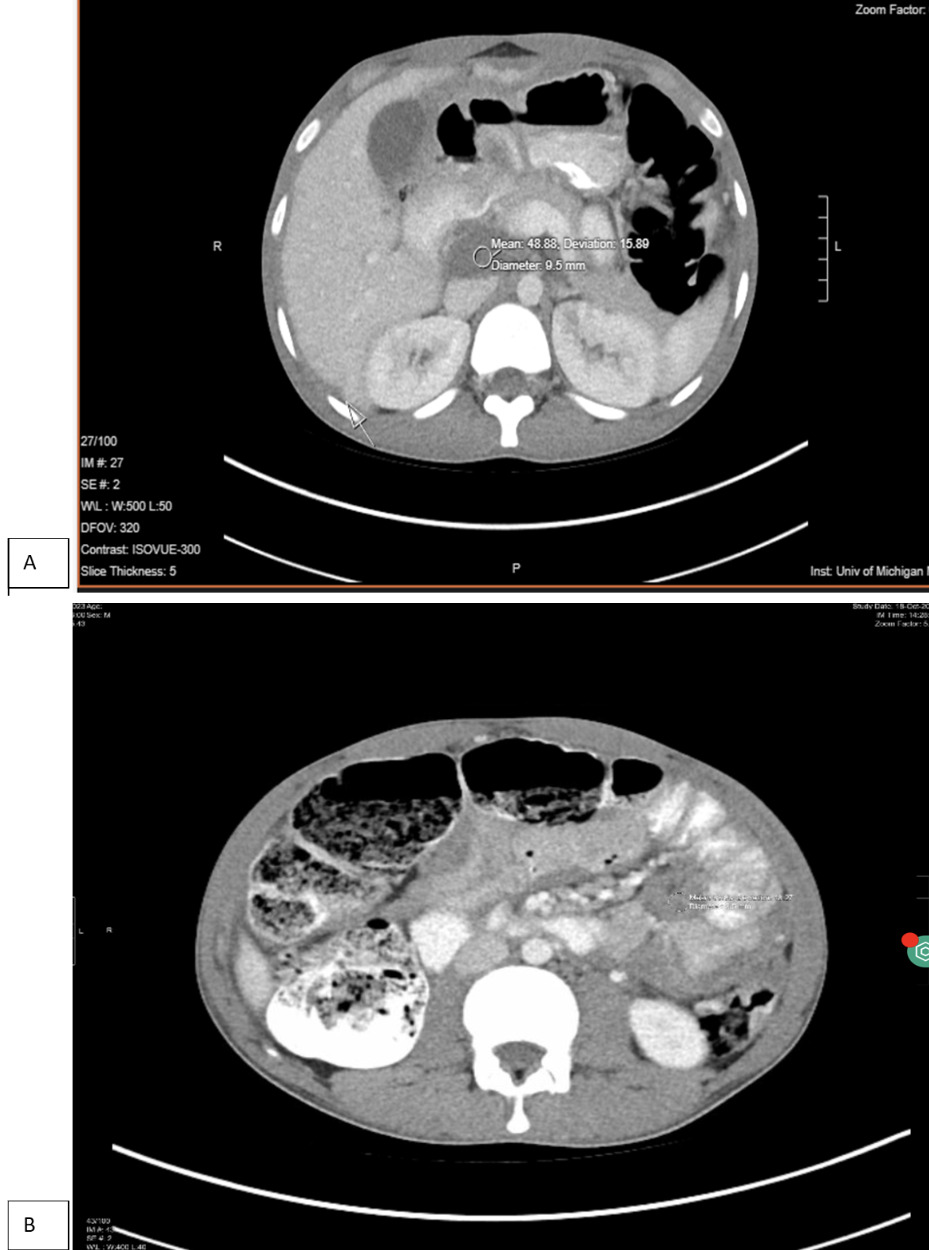
Case Description/Methods: A 22-year-old male, with no significant past medical history who recently immigrated from Yemen, presented with a three-month history of abdominal pain, nausea/vomiting, 20-pound weight loss, intermittent fevers, and night sweats. Laboratory tests showed mild microcytic anemia (Hb 11.2 g/L, MCV 67μm3), elevated ferritin, and low iron and TIBC levels. CT scan showed extensive soft tissue involvement in the mesentery, enlarged porta hepatis lymph node, mass on bowel loops and liver metastases suggesting peritoneal malignancy spread such as lymphoma (Figure 1). Biopsy revealed necrotizing granulomatous inflammation. Further workup included negative fungal culture, AFB sputum culture smear and MTB PCR, AFB blood culture. An abdominal tissue culture was positive for M. Tuberculosis, and a positive Quant TB test confirmed the diagnosis of tuberculosis.
Discussion: Tuberculosis can affect the GI system most commonly the leocaecal region and is the sixth most common site of extrapulmonary TB. Bacteria reach the GI tract via hematogenous spread, ingestion of infected sputum, or direct spread from adjacent areas. Pathological features include ulcers, fibrosis, bowel wall and omental thickening, enlarged lymph nodes and peritoneal tubercles. Peritoneal TB presents in three forms: wet with ascites, dry with adhesions, and fibrotic with omental thickening. Usually presenting with a lower abdominal pain, palpable mass or complications like perianal fistulae, obstruction, perforation, or malabsorption. Only 25% of cases show pulmonary lesions. Ascitic fluid analysis shows high protein, low SAAG, lymphocytic cells, and elevated ADA. Treatment involves at least six months of antitubercular therapy.
This case highlights the diagnostic complexities associated with extrapulmonary abdominal tuberculosis, emphasizing the necessity for heightened clinical suspicion in high risk populations such as immigrants, immunocompromised individuals, and travelers to endemic regions. It also emphasizes the potential discordance between radiological findings and definitive diagnosis, highlighting the risk of anchoring bias. Maintaining a broad differential diagnosis early in the evaluation process can help minimize anchoring bias
Disclosures:
Haya Omeish, MD1, Aaron Berg, MD2, Maximilian Von Hohenberg, MD2, Husam Bader, MD2. P4953 - Abdominal Imaging Versus Tissue Biopsy: A Challenging Case of Abdominal TB, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2University of Michigan, Ann Arbor, MI
Introduction: Tuberculosis, caused by Mycobacterium tuberculosis, remains one of the leading infectious causes of death worldwide. It is classified as either pulmonary or extrapulmonary. The gastrointestinal system involvement in tuberculosis is rare.
Case Description/Methods: A 22-year-old male, with no significant past medical history who recently immigrated from Yemen, presented with a three-month history of abdominal pain, nausea/vomiting, 20-pound weight loss, intermittent fevers, and night sweats. Laboratory tests showed mild microcytic anemia (Hb 11.2 g/L, MCV 67μm3), elevated ferritin, and low iron and TIBC levels. CT scan showed extensive soft tissue involvement in the mesentery, enlarged porta hepatis lymph node, mass on bowel loops and liver metastases suggesting peritoneal malignancy spread such as lymphoma (Figure 1). Biopsy revealed necrotizing granulomatous inflammation. Further workup included negative fungal culture, AFB sputum culture smear and MTB PCR, AFB blood culture. An abdominal tissue culture was positive for M. Tuberculosis, and a positive Quant TB test confirmed the diagnosis of tuberculosis.
Discussion: Tuberculosis can affect the GI system most commonly the leocaecal region and is the sixth most common site of extrapulmonary TB. Bacteria reach the GI tract via hematogenous spread, ingestion of infected sputum, or direct spread from adjacent areas. Pathological features include ulcers, fibrosis, bowel wall and omental thickening, enlarged lymph nodes and peritoneal tubercles. Peritoneal TB presents in three forms: wet with ascites, dry with adhesions, and fibrotic with omental thickening. Usually presenting with a lower abdominal pain, palpable mass or complications like perianal fistulae, obstruction, perforation, or malabsorption. Only 25% of cases show pulmonary lesions. Ascitic fluid analysis shows high protein, low SAAG, lymphocytic cells, and elevated ADA. Treatment involves at least six months of antitubercular therapy.
This case highlights the diagnostic complexities associated with extrapulmonary abdominal tuberculosis, emphasizing the necessity for heightened clinical suspicion in high risk populations such as immigrants, immunocompromised individuals, and travelers to endemic regions. It also emphasizes the potential discordance between radiological findings and definitive diagnosis, highlighting the risk of anchoring bias. Maintaining a broad differential diagnosis early in the evaluation process can help minimize anchoring bias
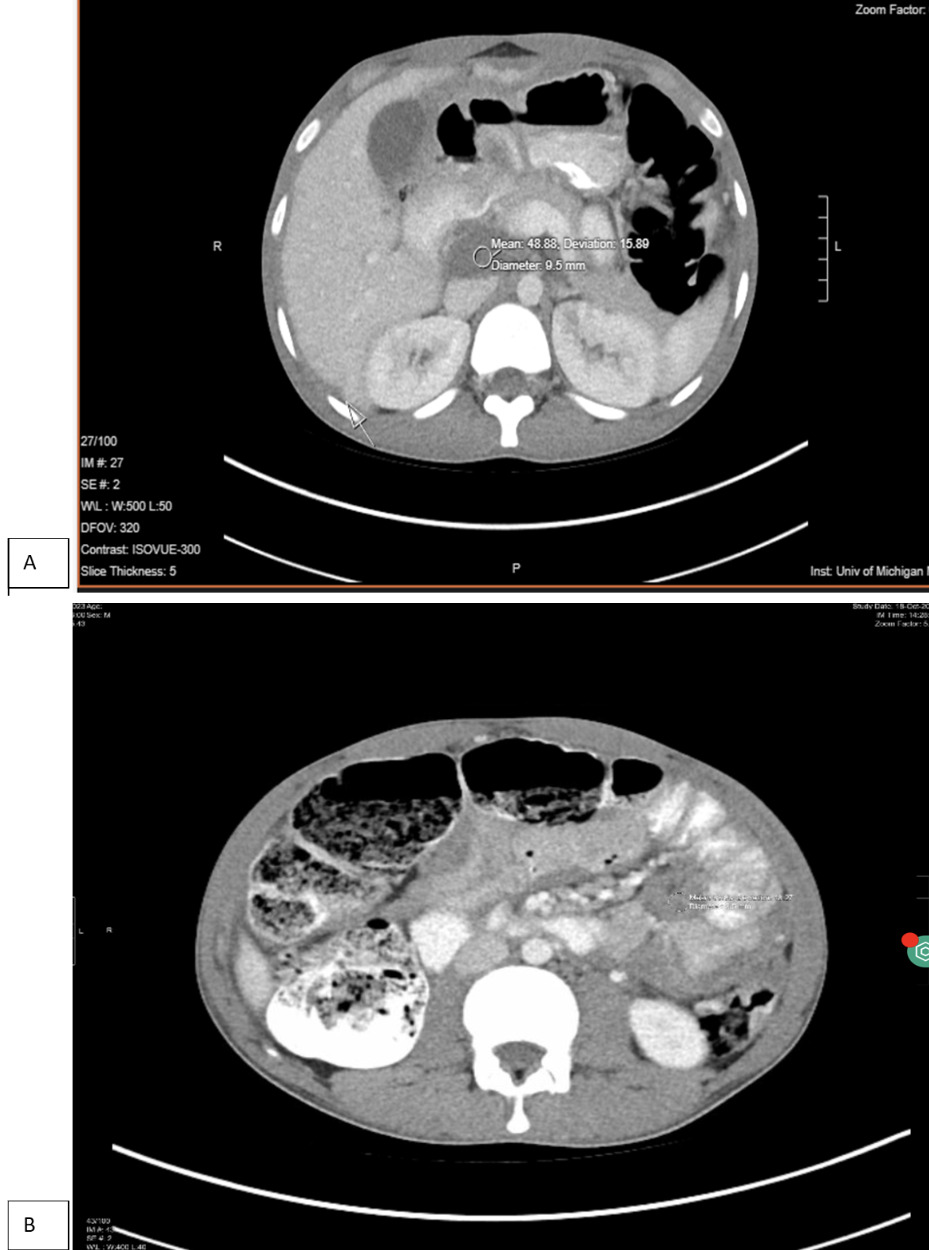
Figure: Figure-1- (A) imaging initially suggestive of lymphoma (B) Extra-pulmonary TB with diffuse mesenteric soft tissue nodularity, hepatic lesions and enlarged porta hepatis lymph node.
Disclosures:
Haya Omeish indicated no relevant financial relationships.
Aaron Berg indicated no relevant financial relationships.
Maximilian Von Hohenberg indicated no relevant financial relationships.
Husam Bader indicated no relevant financial relationships.
Haya Omeish, MD1, Aaron Berg, MD2, Maximilian Von Hohenberg, MD2, Husam Bader, MD2. P4953 - Abdominal Imaging Versus Tissue Biopsy: A Challenging Case of Abdominal TB, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
