Tuesday Poster Session
Category: Small Intestine
P4976 - Marginal Cell Lymphoma: A Rare Presentation of Gastric Outlet Obstruction
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio
- IT
Ian Tobal, DO
Ochsner Medical Center
Jefferson, LA
Presenting Author(s)
Ian Tobal, DO1, James Gore, DO2, Paula Cacioppo, MD2, Timothy Goyette, MD1, Ernest Philon, DO1
1Ochsner Medical Center, Jefferson, LA; 2Ochsner Health Clinic Foundation, New Orleans, LA
Introduction: Marginal zone lymphoma, a type of non-Hodgkin lymphoma, is characterized by the clonal expansion of B-cells within the marginal zones of lymphoid tissues. It is a rare subtype, accounting for approximately 10-20% of all lymphomas, usually occurring in sites such as the stomach, ocular adnexa, and lung. While the exact cause is unclear, it has been associated with chronic infections such as Helicobacter pylori, autoimmune disorders, and environmental factors.
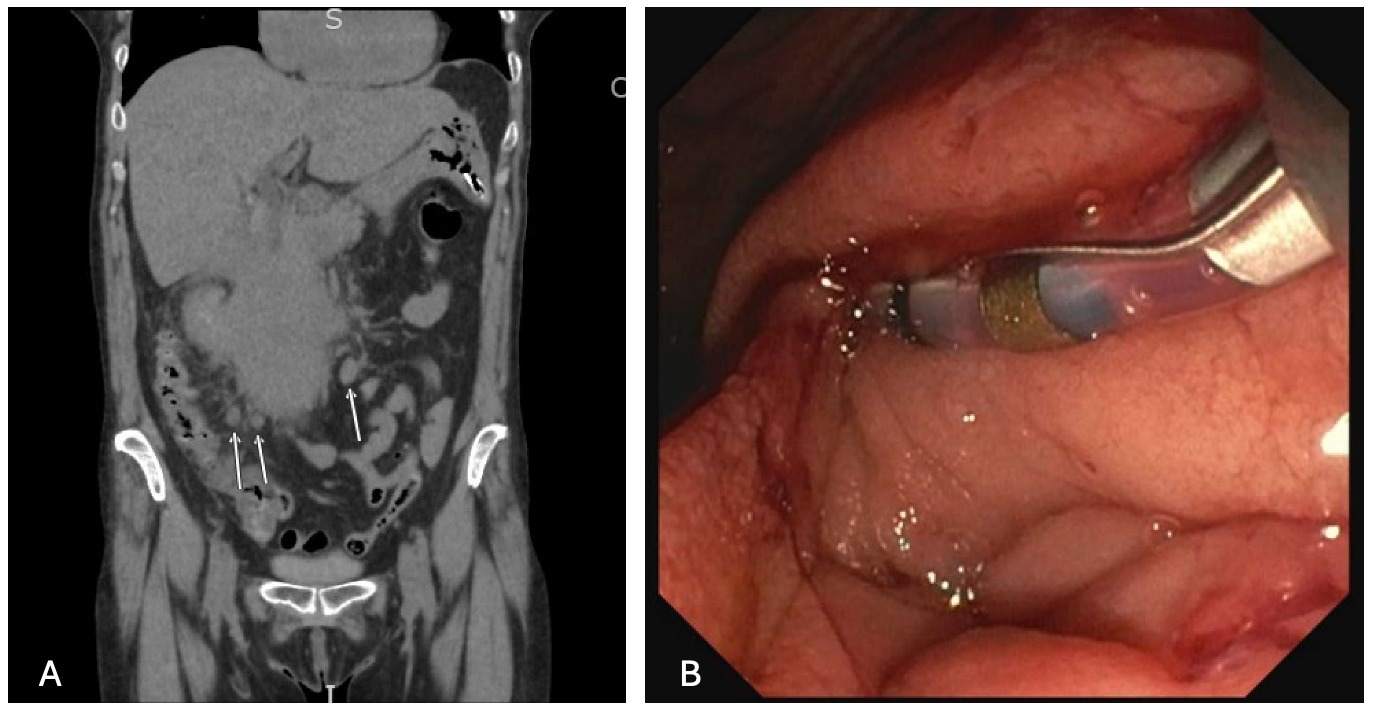
Case Description/Methods: A 60-year-old female with a history of tobacco abuse, cholecystectomy, and eppendectomy presented with a 4-month history of diffuse abdominal pain, worse in the upper abdomen, along with a 20 lb weight loss. She also reported occasional night sweats, fever, and chills. Over the previous several days, she had been unable to tolerate solid or liquid food due to persistent vomiting. Laboratory workup was notable for leukocytosis with WBC 21.79 and microcytic anemia with Hgb 8.9. CT Abdomen and Pelvis showed a massive (10.2 x 7.3 x 5.9 cm) heterogeneous pancreatic head mass with possible invasion to the duodenum with mild upstream obstruction, invasion of the IVC, and potential invasion upon the right kidney with associated hydronephrosis.
EGD revealed a complete duodenal obstruction. EUS with multiple biopsies was obtained. Flow cytometry was suggestive of DLBCL, high-grade follicular lymphoma, marginal zone lymphoma, and lymphoplasmacytic lymphoma.
She was placed on a pulse dose of dexamethasone (20mg daily for 4 days) followed by R-CHOP (a chemotherapy regimen including cyclophosphamide, doxorubicin hydrochloride, vincristine, rituximab, and prednisone. The nasogastric tube was eventually removed and the patient was started on a clear liquid diet. The leukocytosis improved with broad-spectrum antibiotics.
Discussion: In a patient with a history of multiple intra-abdominal surgeries, it can be convenient to attribute an SBO to adhesions or other common causes such as hernias. A systematic review has shown that neoplasms only account for roughly 5% of this disorder. Although rare, marginal cell lymphoma should remain in the differential diagnosis for SBO and small bowel strictures. While an uncommon presentation of marginal cell lymphoma, this case reminds us of the importance of adequate tissue sampling to clarify diagnosis. Detection and identification of marginal zone lymphoma is crucial for improved diagnosis and management of this lymphoma subtype.
Disclosures:
Ian Tobal, DO1, James Gore, DO2, Paula Cacioppo, MD2, Timothy Goyette, MD1, Ernest Philon, DO1. P4976 - Marginal Cell Lymphoma: A Rare Presentation of Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Ochsner Medical Center, Jefferson, LA; 2Ochsner Health Clinic Foundation, New Orleans, LA
Introduction: Marginal zone lymphoma, a type of non-Hodgkin lymphoma, is characterized by the clonal expansion of B-cells within the marginal zones of lymphoid tissues. It is a rare subtype, accounting for approximately 10-20% of all lymphomas, usually occurring in sites such as the stomach, ocular adnexa, and lung. While the exact cause is unclear, it has been associated with chronic infections such as Helicobacter pylori, autoimmune disorders, and environmental factors.
Case Description/Methods: A 60-year-old female with a history of tobacco abuse, cholecystectomy, and eppendectomy presented with a 4-month history of diffuse abdominal pain, worse in the upper abdomen, along with a 20 lb weight loss. She also reported occasional night sweats, fever, and chills. Over the previous several days, she had been unable to tolerate solid or liquid food due to persistent vomiting. Laboratory workup was notable for leukocytosis with WBC 21.79 and microcytic anemia with Hgb 8.9. CT Abdomen and Pelvis showed a massive (10.2 x 7.3 x 5.9 cm) heterogeneous pancreatic head mass with possible invasion to the duodenum with mild upstream obstruction, invasion of the IVC, and potential invasion upon the right kidney with associated hydronephrosis.
EGD revealed a complete duodenal obstruction. EUS with multiple biopsies was obtained. Flow cytometry was suggestive of DLBCL, high-grade follicular lymphoma, marginal zone lymphoma, and lymphoplasmacytic lymphoma.
She was placed on a pulse dose of dexamethasone (20mg daily for 4 days) followed by R-CHOP (a chemotherapy regimen including cyclophosphamide, doxorubicin hydrochloride, vincristine, rituximab, and prednisone. The nasogastric tube was eventually removed and the patient was started on a clear liquid diet. The leukocytosis improved with broad-spectrum antibiotics.
Discussion: In a patient with a history of multiple intra-abdominal surgeries, it can be convenient to attribute an SBO to adhesions or other common causes such as hernias. A systematic review has shown that neoplasms only account for roughly 5% of this disorder. Although rare, marginal cell lymphoma should remain in the differential diagnosis for SBO and small bowel strictures. While an uncommon presentation of marginal cell lymphoma, this case reminds us of the importance of adequate tissue sampling to clarify diagnosis. Detection and identification of marginal zone lymphoma is crucial for improved diagnosis and management of this lymphoma subtype.
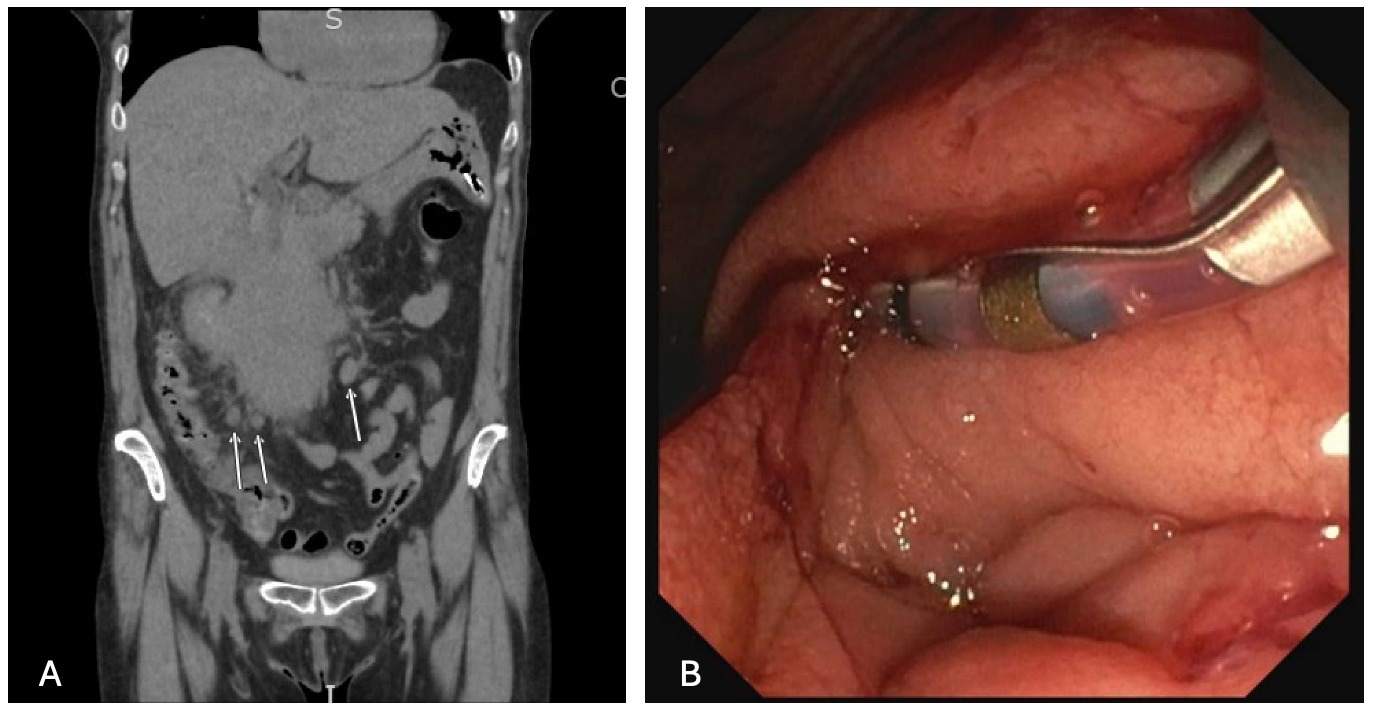
Figure: A) Coronal CT image of the mass with surrounding mesenteric inflammatory change. Arrows pointing to abnormal regional lymph nodes.
B) ERCP image showing complete duodenal obstruction.
B) ERCP image showing complete duodenal obstruction.
Disclosures:
Ian Tobal indicated no relevant financial relationships.
James Gore indicated no relevant financial relationships.
Paula Cacioppo indicated no relevant financial relationships.
Timothy Goyette indicated no relevant financial relationships.
Ernest Philon indicated no relevant financial relationships.
Ian Tobal, DO1, James Gore, DO2, Paula Cacioppo, MD2, Timothy Goyette, MD1, Ernest Philon, DO1. P4976 - Marginal Cell Lymphoma: A Rare Presentation of Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
