Tuesday Poster Session
Category: Small Intestine
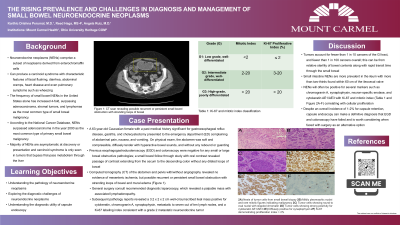
P4992 - The Rising Prevalence and Challenges in Diagnosis and Management of Small Bowel Neuroendocrine Neoplasms
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Karthic Drishna Perumal, MD
Mount Carmel Health System, OH
Presenting Author(s)
Karthic Drishna Perumal, MD1, Reed Haga, 2, Angela Ruiz, MD3
1Mount Carmel Health System, Powell, OH; 2Heritage College of Osteopathic Medicine, Ohio University, Grove City, OH; 3Mount Carmel Health System, Grove City, OH
Introduction: Neuroendocrine neoplasms (NENs) comprise a subset of neoplasms derived from enterochromaffin cells that are often defined by the potent bioactive amine products secreted to produce a carcinoid syndrome (CS). However, CS is only seen in tumors that bypass first-pass metabolism through the liver and direct release of secretory products into the systemic circulation. Thus, primary NENs of the midgut are particularly challenging to manage and diagnose since symptom presentation can range from nonspecific and vague abdominal pain to partial bowel obstruction.
Case Description/Methods: We present a 63-year-old Caucasian female with a past medical history significant for gastroesophageal reflux disease, gastritis, prior cholecystectomy, who presented to the emergency department (ED) complaining of abdominal pain, nausea, and vomiting. She continued to have bowel movements and passage of flatus, without any fevers, chills, unintentional weight loss, chest pain, shortness of breath, dysuria, hematemesis, tenesmus, or hematochezia. Computed tomography (CT) of the abdomen demonstrated recurrent or persistent small bowel obstruction with stranding loops of bowel. Eventually a diagnostic laparoscopy converted to open small bowel resection with primary anastomosis revealed a palpable mass with associated lymphadenopathy. Pathology reports revealed a 3.2 x 2 x 2 cm well-circumscribed ileal mass that stained positive via immunohistochemical studies for a grade 2 metastatic neuroendocrine tumor.
Discussion: One of the rarer causes of small bowel obstruction are tumors, as they account for fewer than 1 in 10 cancers of the GI tract, and fewer than 1 in 100 cancers overall. The primary tumor is often difficult to visualize even with modern imaging modalities and histopathological evaluation remains paramount in definitive diagnosis. Our patient underwent multiple imaging modality studies that yielded no significant diagnostic causes of her abdominal pain. She eventually progressed to a diagnostic laparoscopy and small bowel resection, in which immunohistochemical staining positive for cytokeratin, chromogranin A, synaptophysin ultimately gave the definitive diagnosis of a small bowel NEN. Capsule endoscopy was considered high risk for retention from stricture due to previous studies suggesting Crohn's/regional enteritis, but can be considered in future cases since the risk of post-surgical adhesions themselves carry high risks for future episodes of small bowel obstruction.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Karthic Drishna Perumal, MD1, Reed Haga, 2, Angela Ruiz, MD3. P4992 - The Rising Prevalence and Challenges in Diagnosis and Management of Small Bowel Neuroendocrine Neoplasms, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Carmel Health System, Powell, OH; 2Heritage College of Osteopathic Medicine, Ohio University, Grove City, OH; 3Mount Carmel Health System, Grove City, OH
Introduction: Neuroendocrine neoplasms (NENs) comprise a subset of neoplasms derived from enterochromaffin cells that are often defined by the potent bioactive amine products secreted to produce a carcinoid syndrome (CS). However, CS is only seen in tumors that bypass first-pass metabolism through the liver and direct release of secretory products into the systemic circulation. Thus, primary NENs of the midgut are particularly challenging to manage and diagnose since symptom presentation can range from nonspecific and vague abdominal pain to partial bowel obstruction.
Case Description/Methods: We present a 63-year-old Caucasian female with a past medical history significant for gastroesophageal reflux disease, gastritis, prior cholecystectomy, who presented to the emergency department (ED) complaining of abdominal pain, nausea, and vomiting. She continued to have bowel movements and passage of flatus, without any fevers, chills, unintentional weight loss, chest pain, shortness of breath, dysuria, hematemesis, tenesmus, or hematochezia. Computed tomography (CT) of the abdomen demonstrated recurrent or persistent small bowel obstruction with stranding loops of bowel. Eventually a diagnostic laparoscopy converted to open small bowel resection with primary anastomosis revealed a palpable mass with associated lymphadenopathy. Pathology reports revealed a 3.2 x 2 x 2 cm well-circumscribed ileal mass that stained positive via immunohistochemical studies for a grade 2 metastatic neuroendocrine tumor.
Discussion: One of the rarer causes of small bowel obstruction are tumors, as they account for fewer than 1 in 10 cancers of the GI tract, and fewer than 1 in 100 cancers overall. The primary tumor is often difficult to visualize even with modern imaging modalities and histopathological evaluation remains paramount in definitive diagnosis. Our patient underwent multiple imaging modality studies that yielded no significant diagnostic causes of her abdominal pain. She eventually progressed to a diagnostic laparoscopy and small bowel resection, in which immunohistochemical staining positive for cytokeratin, chromogranin A, synaptophysin ultimately gave the definitive diagnosis of a small bowel NEN. Capsule endoscopy was considered high risk for retention from stricture due to previous studies suggesting Crohn's/regional enteritis, but can be considered in future cases since the risk of post-surgical adhesions themselves carry high risks for future episodes of small bowel obstruction.
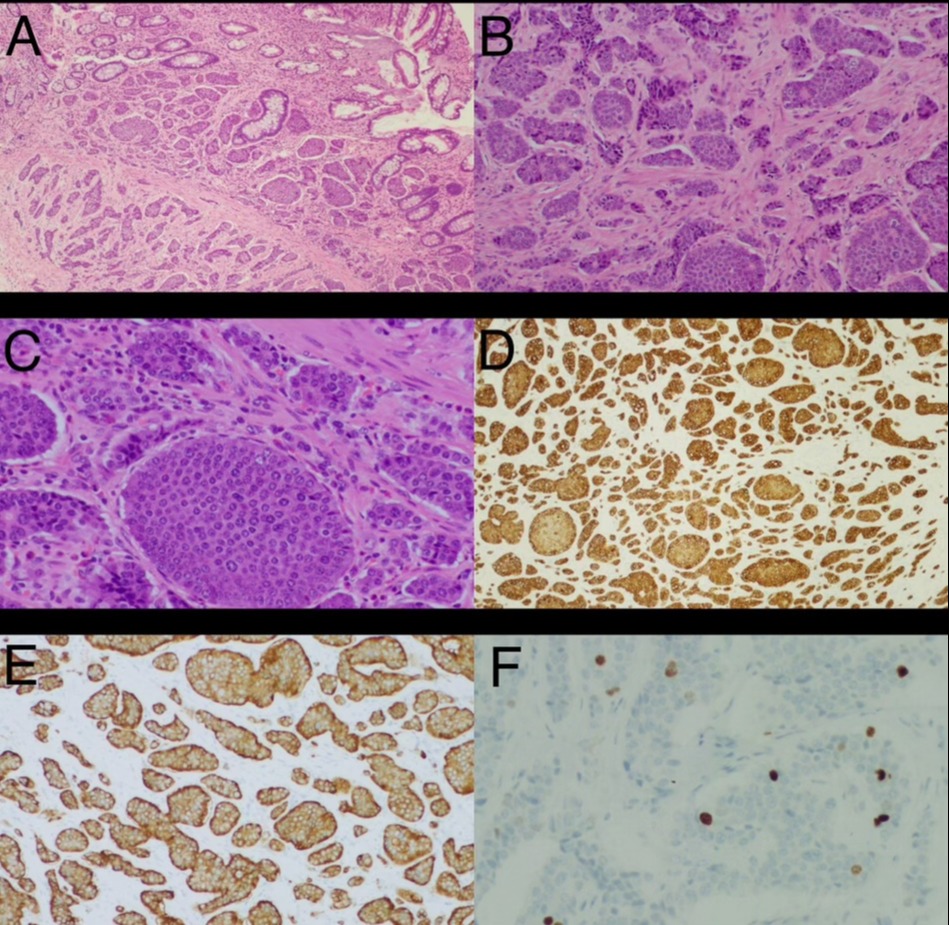
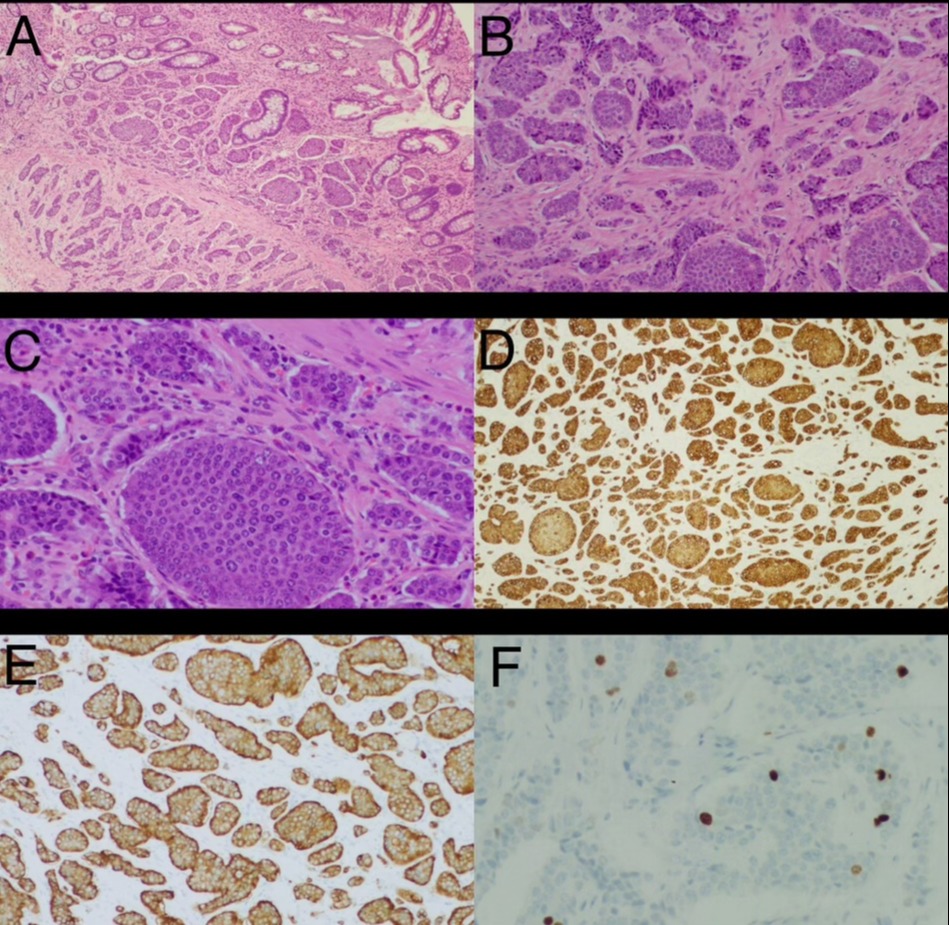
Figure: A) Nests of tumor cells involving small bowel lamina proprietary and submucosa from small bowel biopsy
B) Mildly pleomorphic nuclei and rare mitotic figures indicating malignancy from small bowel biopsy
C) Tumor cells showing round to oval nuclei with stippled chromatin from small bowel biopsy
D) Tumor cells showing strong positivity for cytokeratin AE1/AE3 immunohistochemical staining from small bowel biopsy
E) Diffusely positive Immunostaining for synaptophysin from small bowel biopsy
F) Ki-67 immunohistochemical staining demonstrating proliferation index > 2% from small bowel biopsy
B) Mildly pleomorphic nuclei and rare mitotic figures indicating malignancy from small bowel biopsy
C) Tumor cells showing round to oval nuclei with stippled chromatin from small bowel biopsy
D) Tumor cells showing strong positivity for cytokeratin AE1/AE3 immunohistochemical staining from small bowel biopsy
E) Diffusely positive Immunostaining for synaptophysin from small bowel biopsy
F) Ki-67 immunohistochemical staining demonstrating proliferation index > 2% from small bowel biopsy
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Karthic Drishna Perumal indicated no relevant financial relationships.
Reed Haga indicated no relevant financial relationships.
Angela Ruiz indicated no relevant financial relationships.
Karthic Drishna Perumal, MD1, Reed Haga, 2, Angela Ruiz, MD3. P4992 - The Rising Prevalence and Challenges in Diagnosis and Management of Small Bowel Neuroendocrine Neoplasms, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
