Tuesday Poster Session
Category: Small Intestine
P5008 - From Gut to Brain: A Case of Ataxia in Middle-aged Women With Chronic Diarrhea
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RL
Ramesh Lamichhane, MBBS
Mayo Clinic School of Graduate Medical Education
Rochester, MN
Presenting Author(s)
Ramesh Lamichhane, MBBS, Nicholas R. Oblizajek, MD, Vijay K. Ramanan, MD, PhD
Mayo Clinic School of Graduate Medical Education, Rochester, MN
Introduction: Celiac disease is an immune-mediated disorder of gluten sensitivity primarily affecting the small intestine. Extraintestinal manifestations of the disease can affect nearly any organ system, and although rare, neurological presentations do occur. We present a case of middle-aged woman with progressive gait ataxia ultimately diagnosed with celiac disease, and subsequent slow but remarkable clinical improvement following gluten free lifestyle.
Case Description/Methods: A 42-year-old woman presented with five-month history of worsening gait disturbance, progressing from unremarkable gait to holding herself up via a wall, ultimately to being wheelchair bound. Family history was unremarkable for systemic autoimmune or neurological diseases. Review of systems was only notable for chronically loose stools.
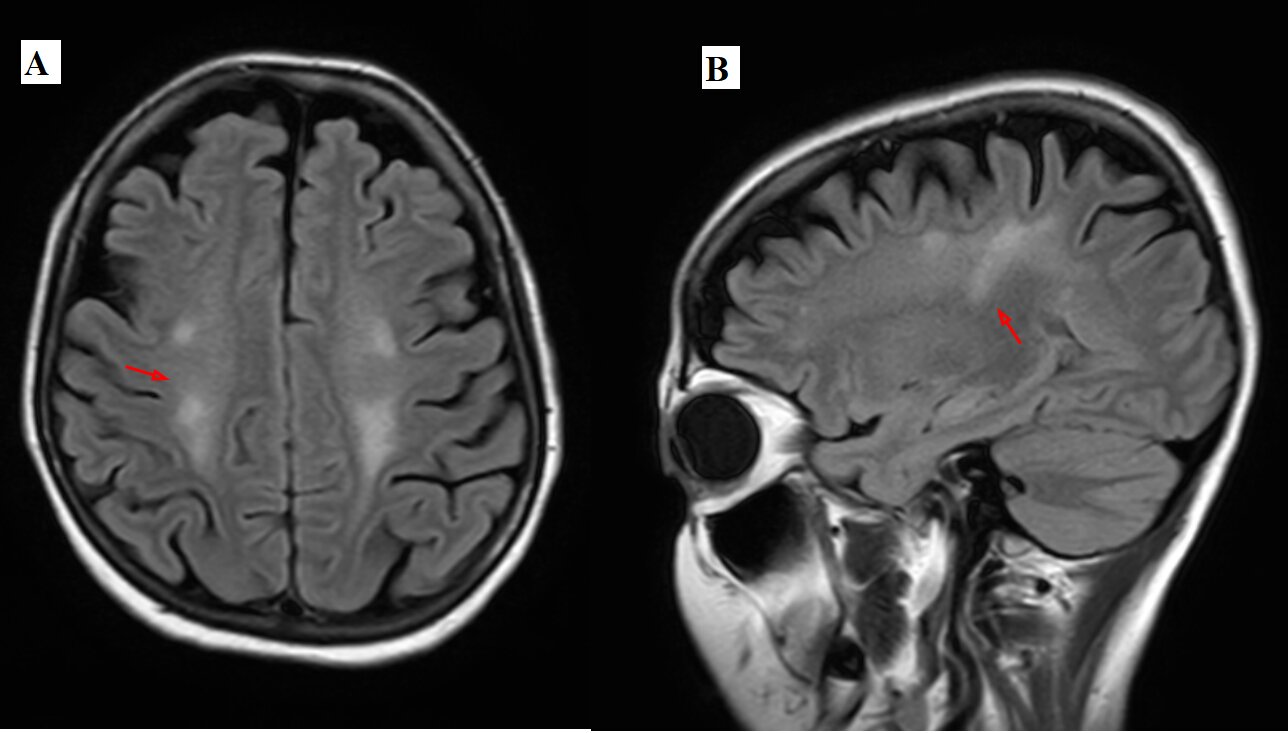
Examination revealed broad based gait, truncal titubation, and appendicular dysmetria. In addition, she had vocal tremor, brisk symmetric reflexes, extensor plantar response, and bilateral non-sustained ankle clonus (4-6 beats). Pertinent laboratory findings are presented in Table 1. MRI brain revealed symmetric T2/FLAIR hyperintensities of both cerebral hemispheres (Figure 1) without abnormality in the cerebellum/brainstem.
Based upon her history of loose stools and multiple nutritional deficiencies, tissue transglutaminase (tTg) serologies with IgA levels were obtained and markedly positive ( >100 U/mL). Confirmatory EGD showed scalloping in the duodenum. Duodenal biopsies confirmed total villous atrophy, increased intraepithelial lymphocytes and crypt hyperplasia. Taken together, the findings were consistent with a diagnosis of celiac disease with gluten ataxia. She was started on a strict gluten-free diet with repletion of deficient vitamins and minerals.
Her symptoms improved significantly although incompletely within 6 months. Over the next three years she continued to improve significantly, with the ability now to ambulate without assistance and independent ascent/descent of stairs.
Discussion: Gluten ataxia classically involves the cerebellum, consistent with this patient’s physical examination, disparate from the MRI findings shown which are likely related to toxic/metabolic changes from vitamin/mineral deficiencies. Copper deficiency myeloneuropathy should be considered, which should almost always include sensory disturbances. The degree of improvement may vary and can continue to improve over years, as seen in this patient.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ramesh Lamichhane, MBBS, Nicholas R. Oblizajek, MD, Vijay K. Ramanan, MD, PhD. P5008 - From Gut to Brain: A Case of Ataxia in Middle-aged Women With Chronic Diarrhea, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic School of Graduate Medical Education, Rochester, MN
Introduction: Celiac disease is an immune-mediated disorder of gluten sensitivity primarily affecting the small intestine. Extraintestinal manifestations of the disease can affect nearly any organ system, and although rare, neurological presentations do occur. We present a case of middle-aged woman with progressive gait ataxia ultimately diagnosed with celiac disease, and subsequent slow but remarkable clinical improvement following gluten free lifestyle.
Case Description/Methods: A 42-year-old woman presented with five-month history of worsening gait disturbance, progressing from unremarkable gait to holding herself up via a wall, ultimately to being wheelchair bound. Family history was unremarkable for systemic autoimmune or neurological diseases. Review of systems was only notable for chronically loose stools.
Examination revealed broad based gait, truncal titubation, and appendicular dysmetria. In addition, she had vocal tremor, brisk symmetric reflexes, extensor plantar response, and bilateral non-sustained ankle clonus (4-6 beats). Pertinent laboratory findings are presented in Table 1. MRI brain revealed symmetric T2/FLAIR hyperintensities of both cerebral hemispheres (Figure 1) without abnormality in the cerebellum/brainstem.
Based upon her history of loose stools and multiple nutritional deficiencies, tissue transglutaminase (tTg) serologies with IgA levels were obtained and markedly positive ( >100 U/mL). Confirmatory EGD showed scalloping in the duodenum. Duodenal biopsies confirmed total villous atrophy, increased intraepithelial lymphocytes and crypt hyperplasia. Taken together, the findings were consistent with a diagnosis of celiac disease with gluten ataxia. She was started on a strict gluten-free diet with repletion of deficient vitamins and minerals.
Her symptoms improved significantly although incompletely within 6 months. Over the next three years she continued to improve significantly, with the ability now to ambulate without assistance and independent ascent/descent of stairs.
Discussion: Gluten ataxia classically involves the cerebellum, consistent with this patient’s physical examination, disparate from the MRI findings shown which are likely related to toxic/metabolic changes from vitamin/mineral deficiencies. Copper deficiency myeloneuropathy should be considered, which should almost always include sensory disturbances. The degree of improvement may vary and can continue to improve over years, as seen in this patient.
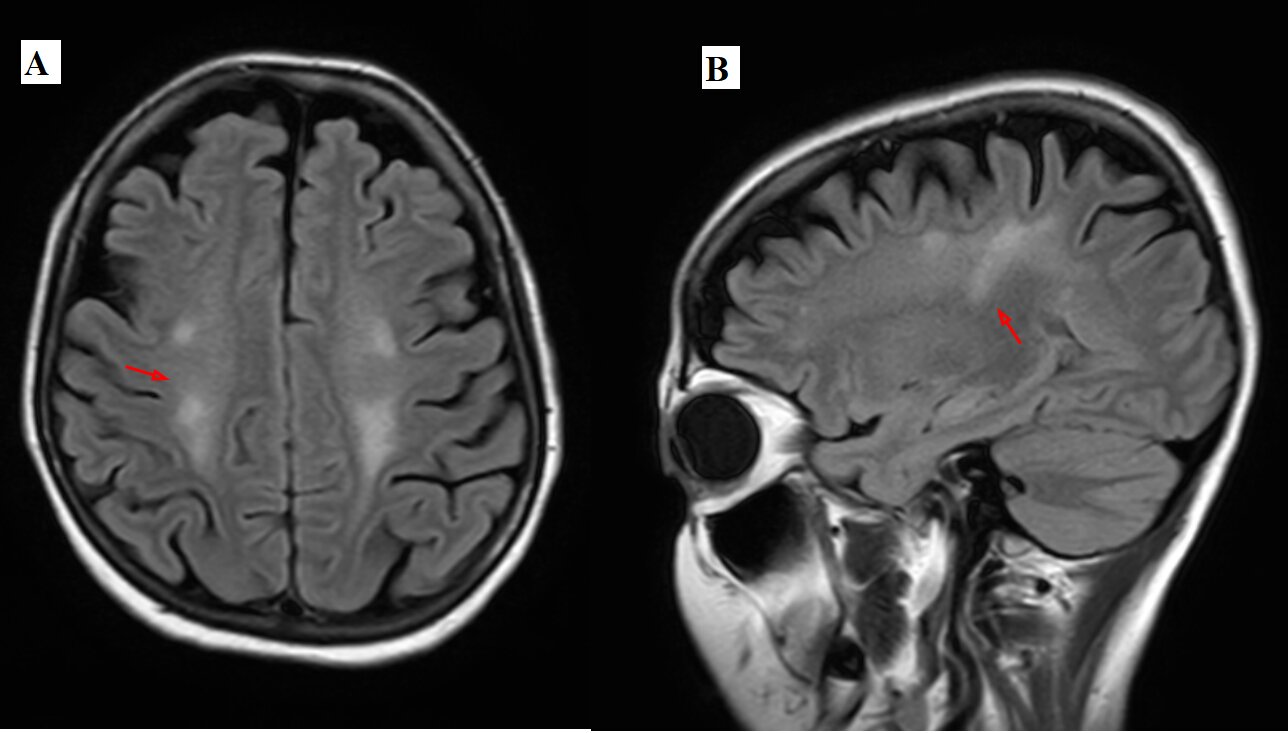
Figure: Figure 1. (Panel A-B) Symmetric T2 hyperintensities involving the subcortical and deep white matter of both cerebral hemispheres, sparing the temporal lobes and periventricular white matter.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ramesh Lamichhane indicated no relevant financial relationships.
Nicholas Oblizajek indicated no relevant financial relationships.
Vijay K. Ramanan: Alzheimer’s Association – Study clinician. Alzheimer’s Clinical Trials Consortium – Study clinician/researcher. Mangurian Foundation for LBD Research – Grant/Research Support. Transposing Therapeutics – Study clinician.
Ramesh Lamichhane, MBBS, Nicholas R. Oblizajek, MD, Vijay K. Ramanan, MD, PhD. P5008 - From Gut to Brain: A Case of Ataxia in Middle-aged Women With Chronic Diarrhea, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
