Tuesday Poster Session
Category: Small Intestine
P5009 - Gut Check: Gastrointestinal Tuberculosis a Potential Mimic of Other Disease
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rhett L. Harmon, MD
Olive View-UCLA Medical Center
Sylmar, CA
Presenting Author(s)
Rhett L. Harmon, MD1, Mark Baniqued, MD2, Soonwook Hong, MD3, Thomas Kovacs, MD1, Shaun Chandna, DO1
1Olive View-UCLA Medical Center, Sylmar, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA
Introduction: Extrapulmonary tuberculosis (EPTB) accounts for 15% of tuberculosis (TB) infections. Predominant sites are abdominal involving the peritoneum and/or intestine. Gastrointestinal (GI) tuberculosis can encompass the entire GI tract, with the ileocecum accounting for 75%. Risk factors include latent TB and immunocompromised status. GI TB can be difficult to diagnose. We report a case of GI TB with ileocolitis, suspected to have peritoneal involvement without active respiratory symptoms.
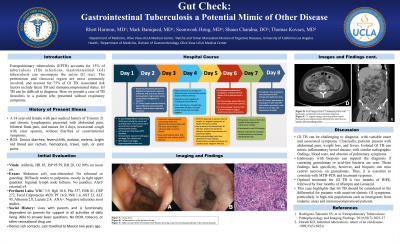
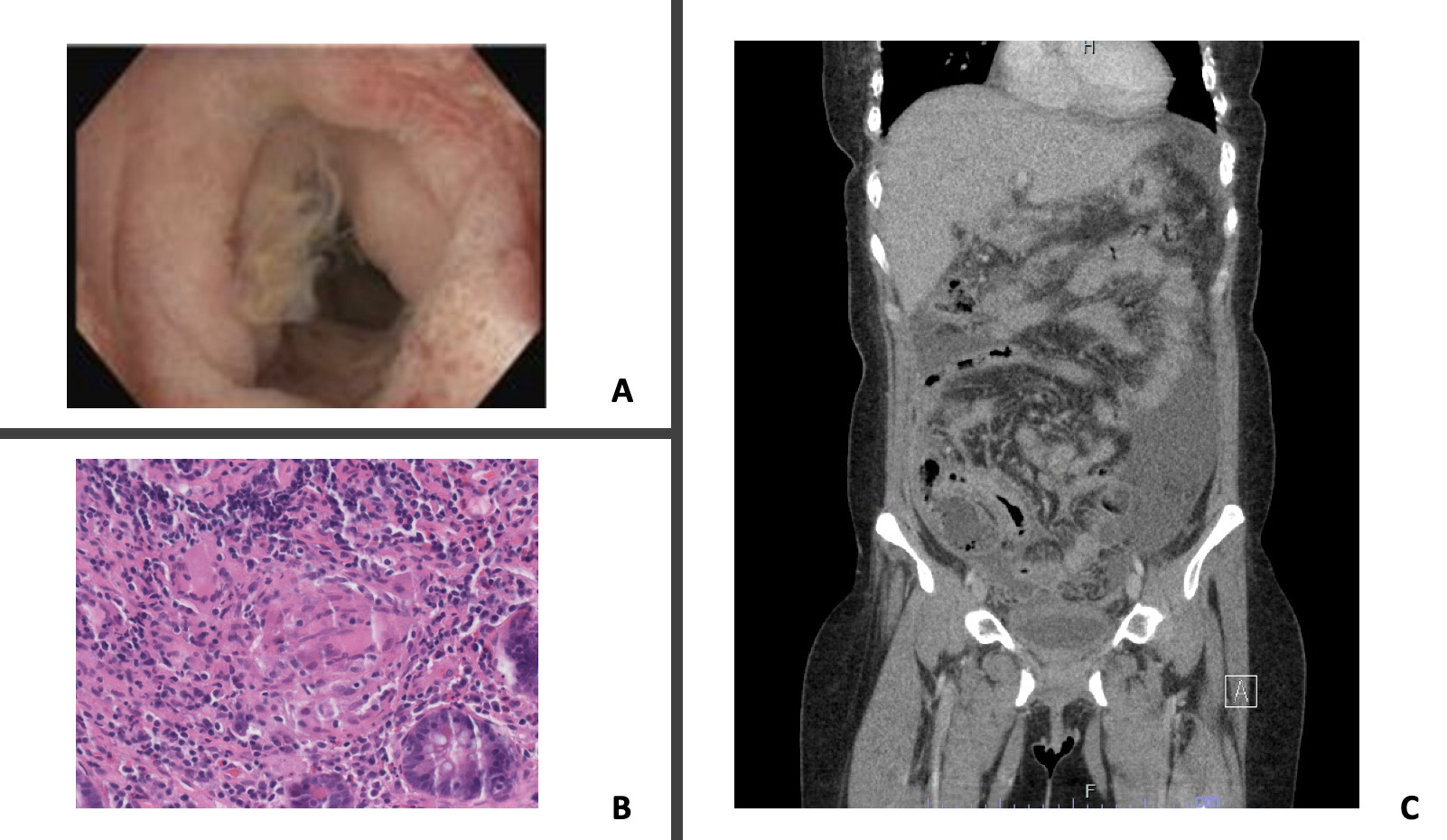
Case Description/Methods: 34 year old female with Trisomy 21 and chronic lymphopenia presented with abdominal pain and nausea for 4 days, occasional cough with clear sputum, without diarrhea or constitutional symptoms. CT abdomen showed diffuse mural thickening of majority of small bowel, cecum, ascending colon most pronounced in terminal ileum, and peritoneal thickening with ascites. Labs showed normal liver tests, low albumin, elevated ESR, CRP, fecal calprotectin, negative infectious stool studies. Paracentesis showed low serum ascites albumin gradient, high protein, negative cytology. CT chest showed pericardial and pleural effusions. Patient had poor response to broad spectrum antibiotics. AFB in sputum and ascites was negative. Sputum mycobacterium TB PCR was positive. Rifampin, isoniazid, ethambutol, pyrazinamide (RIPE) and levofloxacin started. Enteroscopy with colonoscopy revealed terminal ileitis with few ulcers and cecal ulcer. Biopsies respectively showed noncaseating granulomatous ileitis, and focal cryptitis, lymphocytosis, focus suggesting non-caseating granuloma. GI symptoms resolved after treatment initiation.
Discussion: Diagnosis of GI TB can be challenging with variable onset and nonspecific symptoms. Classically, patients present with abdominal pain, weight loss, and fevers. GI TB can mimic inflammatory bowel disease with similar radiographic findings, blood tests, and absence of pulmonary symptoms. Endoscopy with biopsies can support the diagnosis if caseating granulomas or acid-fast bacteria are seen, however these findings lack sensitivity. It is essential to correlate clinically with MTB-PCR and treatment response. Optimal treatment is RIPE for 2 months followed by rifampin and isoniazid for 4 months. Our case of GI TB with suspected peritoneal involvement highlights that GI TB should be considered in the differential for patients with abdominal symptoms, particularly in high-risk populations such as immigrants from endemic areas and immunocompromised patients.
Disclosures:
Rhett L. Harmon, MD1, Mark Baniqued, MD2, Soonwook Hong, MD3, Thomas Kovacs, MD1, Shaun Chandna, DO1. P5009 - Gut Check: Gastrointestinal Tuberculosis a Potential Mimic of Other Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Olive View-UCLA Medical Center, Sylmar, CA; 2David Geffen School of Medicine at UCLA, Los Angeles, CA; 3University of California Los Angeles David Geffen School of Medicine, Los Angeles, CA
Introduction: Extrapulmonary tuberculosis (EPTB) accounts for 15% of tuberculosis (TB) infections. Predominant sites are abdominal involving the peritoneum and/or intestine. Gastrointestinal (GI) tuberculosis can encompass the entire GI tract, with the ileocecum accounting for 75%. Risk factors include latent TB and immunocompromised status. GI TB can be difficult to diagnose. We report a case of GI TB with ileocolitis, suspected to have peritoneal involvement without active respiratory symptoms.
Case Description/Methods: 34 year old female with Trisomy 21 and chronic lymphopenia presented with abdominal pain and nausea for 4 days, occasional cough with clear sputum, without diarrhea or constitutional symptoms. CT abdomen showed diffuse mural thickening of majority of small bowel, cecum, ascending colon most pronounced in terminal ileum, and peritoneal thickening with ascites. Labs showed normal liver tests, low albumin, elevated ESR, CRP, fecal calprotectin, negative infectious stool studies. Paracentesis showed low serum ascites albumin gradient, high protein, negative cytology. CT chest showed pericardial and pleural effusions. Patient had poor response to broad spectrum antibiotics. AFB in sputum and ascites was negative. Sputum mycobacterium TB PCR was positive. Rifampin, isoniazid, ethambutol, pyrazinamide (RIPE) and levofloxacin started. Enteroscopy with colonoscopy revealed terminal ileitis with few ulcers and cecal ulcer. Biopsies respectively showed noncaseating granulomatous ileitis, and focal cryptitis, lymphocytosis, focus suggesting non-caseating granuloma. GI symptoms resolved after treatment initiation.
Discussion: Diagnosis of GI TB can be challenging with variable onset and nonspecific symptoms. Classically, patients present with abdominal pain, weight loss, and fevers. GI TB can mimic inflammatory bowel disease with similar radiographic findings, blood tests, and absence of pulmonary symptoms. Endoscopy with biopsies can support the diagnosis if caseating granulomas or acid-fast bacteria are seen, however these findings lack sensitivity. It is essential to correlate clinically with MTB-PCR and treatment response. Optimal treatment is RIPE for 2 months followed by rifampin and isoniazid for 4 months. Our case of GI TB with suspected peritoneal involvement highlights that GI TB should be considered in the differential for patients with abdominal symptoms, particularly in high-risk populations such as immigrants from endemic areas and immunocompromised patients.
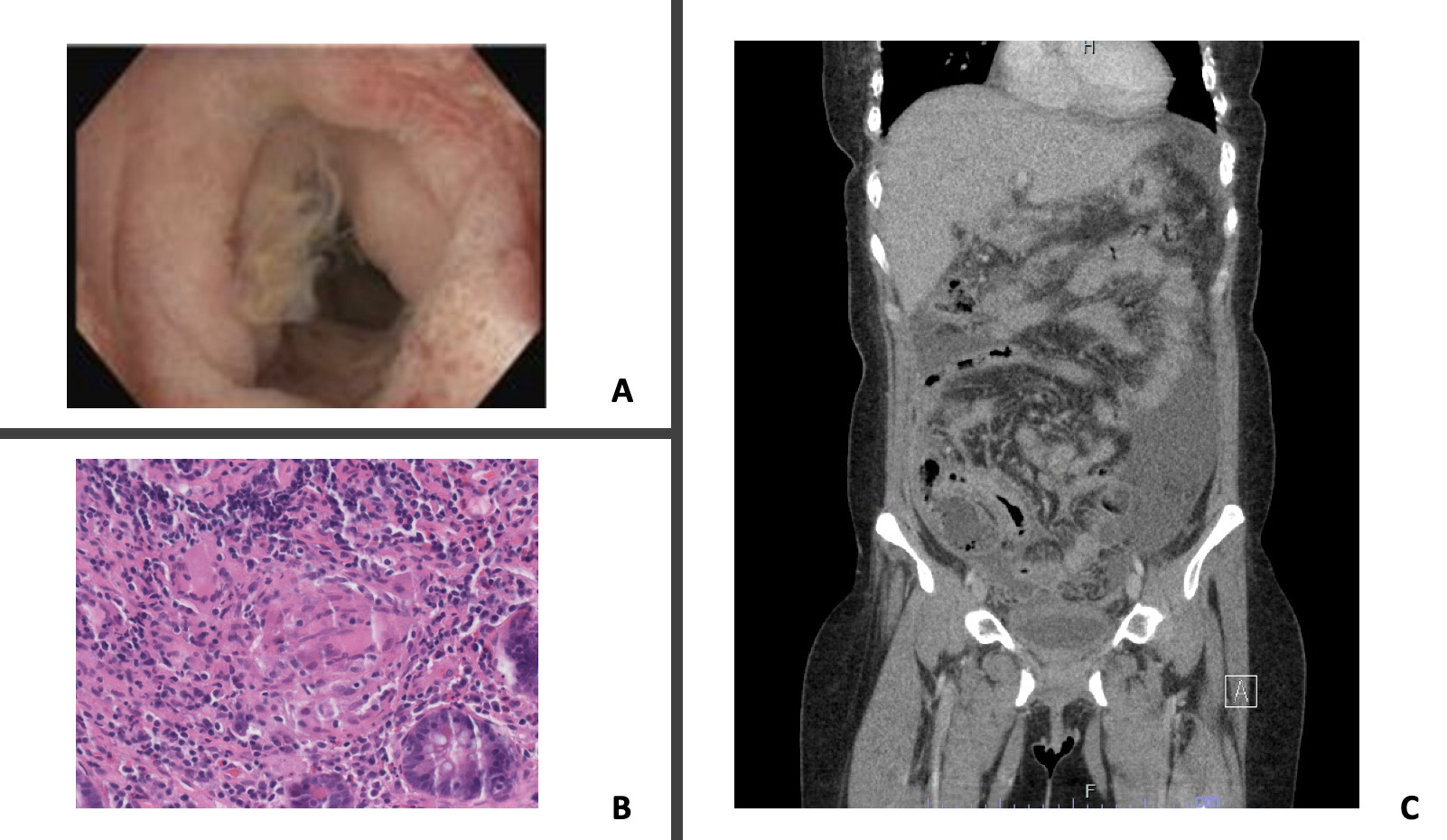
Figure: Figure A: Endoscopic image of Terminal ileitis with scattered ulcers.
Figure B: H&E section (40x) reveals a non-necrotizing granuloma located at the lamina propria consisting of a few multinucleated giant cells and epithelioid histiocytes surrounded by lymphocytes.
Figure C: Coronal CT Abdomen Pelvis depicting diffuse mural thickening and enhancement including the small bowel, cecum, and ascending colon.
Figure B: H&E section (40x) reveals a non-necrotizing granuloma located at the lamina propria consisting of a few multinucleated giant cells and epithelioid histiocytes surrounded by lymphocytes.
Figure C: Coronal CT Abdomen Pelvis depicting diffuse mural thickening and enhancement including the small bowel, cecum, and ascending colon.
Disclosures:
Rhett Harmon indicated no relevant financial relationships.
Mark Baniqued indicated no relevant financial relationships.
Soonwook Hong indicated no relevant financial relationships.
Thomas Kovacs indicated no relevant financial relationships.
Shaun Chandna: Arrowhead Pharmaceuticals – Grant/Research Support. Calliditas Therapeutics (formerly Genkyotex) – Grant/Research Support. Lipocine – Grant/Research Support. Mirum Pharmaceuticals – Grant/Research Support.
Rhett L. Harmon, MD1, Mark Baniqued, MD2, Soonwook Hong, MD3, Thomas Kovacs, MD1, Shaun Chandna, DO1. P5009 - Gut Check: Gastrointestinal Tuberculosis a Potential Mimic of Other Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
