Tuesday Poster Session
Category: Small Intestine
P5018 - Celiac Disease Crisis in a Patient of Peutz-Jeghers Syndrome: An Unusual Coexistence
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shirley Paski, MD, MSc
Staff Gastroenterologist
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Mrigya Sharma, MBBS1, Lady Katherine Mejia Perez, MD2, Shirley Paski, MD, MSc2
1G.M.E.R.S. Medical College, Gotri, Kansas City, KS; 2Cleveland Clinic Foundation, Cleveland, OH
Introduction: Peutz-Jeghers Syndrome (PJS) is a rare genetic disorder caused by STK11 pathogenic variants, characterized by hamartomatous polyps in the gastrointestinal tract and an increased risk of malignancies. Celiac disease, an immune response to gluten, leads to intestinal damage and chronic diarrhea. This report discusses an unusual presentation of celiac crisis in a patient with PJS, highlighting the need to consider common pathologies like celiac disease in patients with rare hereditary disorders presenting with new gastrointestinal symptoms.
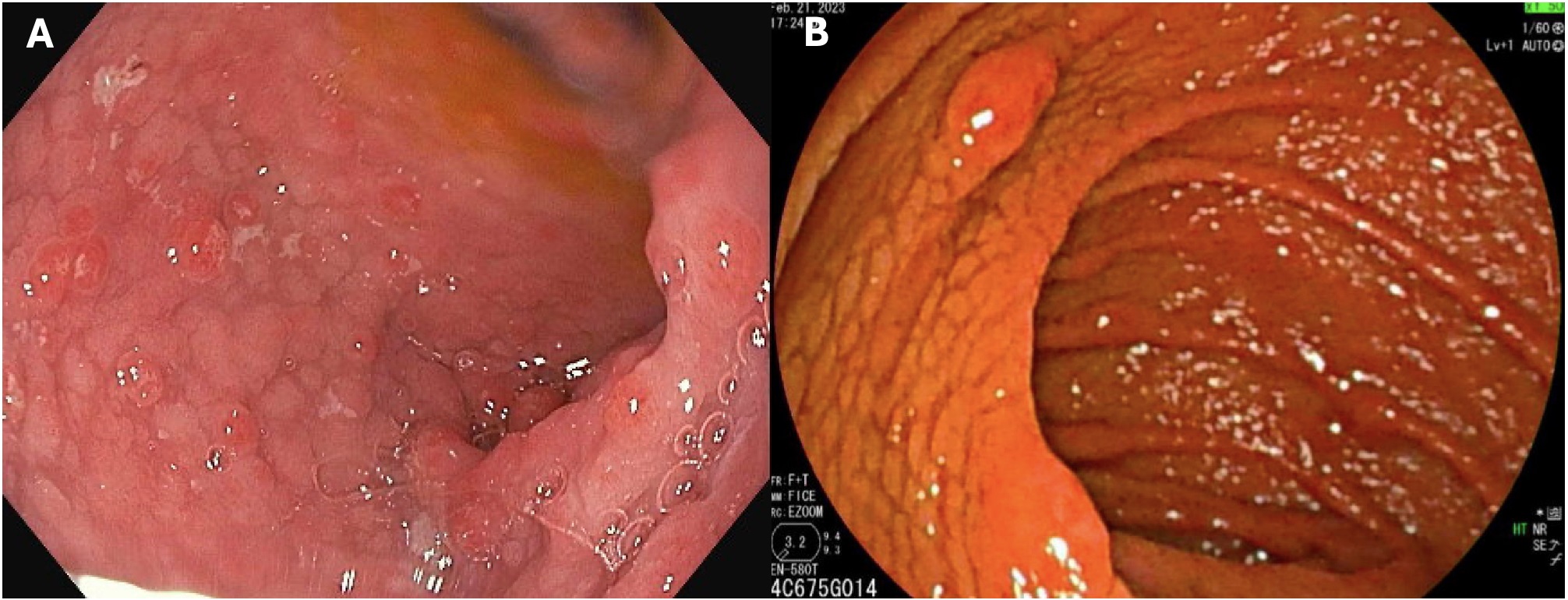
Case Description/Methods: A 38-year-old man with PJS, diagnosed at age 17, presented for endoscopic surveillance. He had a history of multiple surgeries, including small bowel resections for intussusception. Recent imaging had shown 50 small bowel polyps, the largest being 3 cm, and small bowel intussusceptions. Three weeks prior to presentation, he developed severe diarrhea, leading to significant weight loss (17 lbs) and malnutrition. Labs revealed protein-losing enteropathy [1], vitamin and mineral deficiencies. Despite concerns for malignancy due to PJS, further tests indicated elevated transglutaminase IgA and deaminated gliadin IgG. EGD showed nodular duodenal mucosa that was initially felt to be secondary to PJS polyposis (Figure 1.A). Duodenal biopsies showed intraepithelial lymphocytosis and total villous atrophy. A gluten-free diet and budesonide led to significant improvement. He was discharged with plans for follow-up enteroscopy and dietitian referral. Two months later, his symptoms and his malnutrition resolved. Follow-up EGD showed persistent duodenal mucosal cobblestone (Figure 1.B) and pathology showed patchy villous blunting but no intraepithelial lymphocytes, consistent with response to gluten-free diet with lag in villous architecture recovery.
Discussion: The coexistence of PJS and celiac disease is rare and diagnostically challenging. This case emphasizes the importance of a broad differential diagnosis in complex cases. Early diagnosis and management are crucial for improving outcomes and quality of life. This case highlights the need for comprehensive evaluation and maintaining suspicion of common pathologies even in patients with rare hereditary disorders that predispose patients to malignancies.
[1]Bhakta D, Sealock RJ, Hair C. Protein-Losing Enteropathy: An Uncommon Presentation of Celiac Disease. American Journal of Gastroenterology. 2014;109:S316-S317. doi:https://doi.org/10.14309/00000434-201410002-01065
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mrigya Sharma, MBBS1, Lady Katherine Mejia Perez, MD2, Shirley Paski, MD, MSc2. P5018 - Celiac Disease Crisis in a Patient of Peutz-Jeghers Syndrome: An Unusual Coexistence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1G.M.E.R.S. Medical College, Gotri, Kansas City, KS; 2Cleveland Clinic Foundation, Cleveland, OH
Introduction: Peutz-Jeghers Syndrome (PJS) is a rare genetic disorder caused by STK11 pathogenic variants, characterized by hamartomatous polyps in the gastrointestinal tract and an increased risk of malignancies. Celiac disease, an immune response to gluten, leads to intestinal damage and chronic diarrhea. This report discusses an unusual presentation of celiac crisis in a patient with PJS, highlighting the need to consider common pathologies like celiac disease in patients with rare hereditary disorders presenting with new gastrointestinal symptoms.
Case Description/Methods: A 38-year-old man with PJS, diagnosed at age 17, presented for endoscopic surveillance. He had a history of multiple surgeries, including small bowel resections for intussusception. Recent imaging had shown 50 small bowel polyps, the largest being 3 cm, and small bowel intussusceptions. Three weeks prior to presentation, he developed severe diarrhea, leading to significant weight loss (17 lbs) and malnutrition. Labs revealed protein-losing enteropathy [1], vitamin and mineral deficiencies. Despite concerns for malignancy due to PJS, further tests indicated elevated transglutaminase IgA and deaminated gliadin IgG. EGD showed nodular duodenal mucosa that was initially felt to be secondary to PJS polyposis (Figure 1.A). Duodenal biopsies showed intraepithelial lymphocytosis and total villous atrophy. A gluten-free diet and budesonide led to significant improvement. He was discharged with plans for follow-up enteroscopy and dietitian referral. Two months later, his symptoms and his malnutrition resolved. Follow-up EGD showed persistent duodenal mucosal cobblestone (Figure 1.B) and pathology showed patchy villous blunting but no intraepithelial lymphocytes, consistent with response to gluten-free diet with lag in villous architecture recovery.
Discussion: The coexistence of PJS and celiac disease is rare and diagnostically challenging. This case emphasizes the importance of a broad differential diagnosis in complex cases. Early diagnosis and management are crucial for improving outcomes and quality of life. This case highlights the need for comprehensive evaluation and maintaining suspicion of common pathologies even in patients with rare hereditary disorders that predispose patients to malignancies.
[1]Bhakta D, Sealock RJ, Hair C. Protein-Losing Enteropathy: An Uncommon Presentation of Celiac Disease. American Journal of Gastroenterology. 2014;109:S316-S317. doi:https://doi.org/10.14309/00000434-201410002-01065
Figure: A. Initial upper endoscopy revealing cobblestone mucosa and hamartomatous polyps of the duodenal bulb.
B. EGD after treatment with oral budesonide and gluten-free diet revealing scalloped duodenal mucosa, and a hamartomatous polyp.
B. EGD after treatment with oral budesonide and gluten-free diet revealing scalloped duodenal mucosa, and a hamartomatous polyp.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mrigya Sharma indicated no relevant financial relationships.
Lady Katherine Mejia Perez indicated no relevant financial relationships.
Shirley Paski: Cleveland Clinic – Employee. Nutrishare – Advisory Committee/Board Member. Takeda Pharmaceuticals, Inc. – Grant/Research Support.
Mrigya Sharma, MBBS1, Lady Katherine Mejia Perez, MD2, Shirley Paski, MD, MSc2. P5018 - Celiac Disease Crisis in a Patient of Peutz-Jeghers Syndrome: An Unusual Coexistence, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
